Preparing for Postpartum Nutrition After Gestational Diabetes
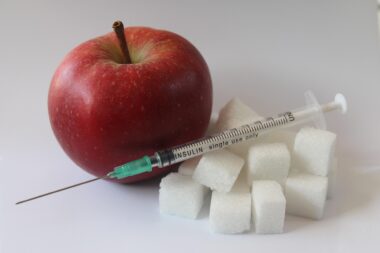
Postpartum nutrition is crucial for new mothers who have experienced gestational diabetes. It influences not just the mother’s well-being but also the health of the newborn. A balanced diet can help mitigate the risks of developing type 2 diabetes later in life. Emphasizing whole foods is essential, with a focus on fruits, vegetables, whole grains, lean proteins, and healthy fats. New mothers should consider their caloric intake, as breastfeeding requires additional energy. Monitoring blood sugar levels is also vital during this phase. Regular meals and snacks can help maintain stable blood sugar levels. It is advisable to consult a healthcare provider or dietitian for personalized meal planning. Maintaining hydration should not be overlooked. Drinking enough water can help improve digestion and boost milk supply. Additionally, avoiding excessive sugars and saturated fats is beneficial for overall health. Including fiber-rich foods can aid digestion and contribute to satiety. Supplements may also be worth discussing with a healthcare professional, especially if dietary restrictions are in place due to gestational diabetes. Adopting these practices sets the foundation for a healthier future.
Understanding the nutrients required post-delivery is paramount for effective recovery. Essential vitamins and minerals such as iron, calcium, and folic acid support healing and enhance energy levels. Lean meats, leafy greens, nuts, and seeds should be included in daily meals. Incorporating a variety of colors in meals typically indicates nutrient diversity, which is beneficial. New mothers should also prioritize protein, which is vital for muscle repair and overall recovery. Foods such as poultry, fish, beans, and legumes can help meet protein needs. Whole grain carbohydrates provide necessary energy to cope with the demands of motherhood and recovery. It’s important to recognize that meal prepping can also enhance nutritional choices. This might involve planning meals ahead or batch-cooking healthy options to ensure nutrient-rich selections are readily available. Keeping healthy snacks on hand is helpful for busy schedules. Furthermore, engaging family members in meal preparation can foster support and healthy eating habits. Lastly, mothers should not hesitate to reach out for emotional support, acknowledging that mental well-being impacts physical health. Equally, forming a support group with other new mothers often brings encouragement and shared experiences.
Creating a Balanced Meal Plan
When developing a postpartum nutrition plan, balance is key to effective recovery. A typical meal should include a source of protein, healthy fat, and carbohydrates. Adhering to the MyPlate guidelines can simplify meal planning, focusing on portion sizes and nutrient density. Portions can vary depending on individual needs, activity levels, and dietary preferences. Starting with about a quarter of the plate filled with lean proteins, a quarter with whole grains, and half with fruits and vegetables creates balance. Additionally, healthy fats like avocados, nuts, and olive oil should be included, supporting heart health. Consider introducing meal schedules or routine times for eating to establish consistency. This will also help balance blood sugar levels throughout the day. Healthy snacks are essential between meals; options like yogurt with berries, mixed nuts, or hummus with veggies can work wonders. This results in sustained energy levels and fewer cravings. Meal planning applications can assist in customizing and tracking nutrient intake. Consulting with a dietitian can further refine the plan, ensuring it meets personal preferences and dietary restrictions. Having a structured approach can significantly improve the transition into this new chapter of motherhood.
Hydration plays a vital role in postpartum nutrition, particularly for breastfeeding mothers. Adequate fluid intake is crucial for maintaining milk production and overall health. Water is the best source of hydration, but other options like herbal teas and infused water can add variety. Mothers should aim for at least eight to ten cups of fluids per day, or more if active or living in a hot climate. Monitoring hydration can be easily done by observing thirst signals and urinary color. Inadequate hydration may lead to fatigue and decreased milk supply, complicating postpartum recovery. High-water-content fruits and vegetables, such as cucumbers, watermelon, and oranges, can contribute to daily fluid intake effectively. Additionally, caffeinated beverages, such as coffee or tea, should be consumed in moderation, as excessive caffeine may impact both hydration and baby’s sleep. Avoiding sugary drinks, like soda or sweetened teas, is also advisable due to their lack of nutritional value and impact on blood sugar levels. Lastly, keeping a reusable water bottle handy throughout the day serves as a reminder to hydrate. Consistent hydration can significantly enhance recovery experiences, providing energy and improving overall health.
Managing Emotional Well-Being
Emotional well-being is as critical as physical health when it comes to postpartum recovery. New mothers may experience a range of emotions, from joy to anxiety, particularly if gestational diabetes was a concern during pregnancy. Recognizing these feelings is a healthy first step toward managing them. Support systems play a vital role; connecting with family or friends can help mitigate feelings of isolation. Consider joining a parenting group or class to foster connections with other new mothers experiencing similar challenges. Practicing self-care, such as taking time for hobbies or quiet moments, nurtures mental health. Engaging in relaxation techniques like deep breathing or meditation can also ease stress and enhance emotional resilience. Especially beneficial can be exercise, which releases endorphins and boosts mood. Simple activities, like walking or yoga, can fit seamlessly into a new mother’s schedule. Prioritize sleep by creating a sleep schedule that aligns with the baby’s. Lastly, avoid perfectionism; embrace the notion of “good enough” during this transitional phase. Seeking help from professionals such as counselors can provide additional support to manage these emotional complexities effectively. Maintaining a balanced emotional state benefits both mother and baby.
Meal preparation strategies can ease the burden of postpartum nutrition planning. Preparing meals in advance and creating a rotating menu can make it easier to maintain a balanced diet. Engaging a partner or family member to assist in meal prep can enhance this experience, fostering togetherness in the kitchen. Create a list focusing on nutrient-dense ingredients and seasonal produce, ensuring freshness. Batch-cooking meals can save time and effort; consider preparing stews, soups, and casseroles that reheat well. Storing pre-portioned meals in the freezer allows for convenient access on busy days. Utilize slow cookers or Instant Pots to simplify meal preparation even further, making it easy to create healthy dishes from scratch. Incorporate leafy greens and various colorful vegetables into meals, maximizing nutrient intake. Don’t forget to label containers with dates to avoid confusion. Also, take advantage of online grocery delivery services, which can save time and enhance convenience. Having healthy options available at home makes it easier to resist unhealthy cravings. Formulating these strategies can significantly contribute to a new mother’s health, laying a foundation for a more manageable postpartum period. Effective planning ensures that nutrition remains a priority amid new motherhood’s demands.
Long-Term Health Considerations
Postpartum nutrition can have lasting effects, influencing long-term health outcomes for mothers who experienced gestational diabetes. Continuing to adopt a balanced diet may help decrease the likelihood of developing type 2 diabetes in the future. New mothers should remain aware of their body’s changes and prioritize regular check-ups with healthcare professionals. Testing glucose levels post-delivery is essential for understanding individual risks better and managing overall health. Emphasizing lifelong nutrition habits is beneficial – focus on incorporating more plant-based foods, reducing processed items, and opting for whole grains. Staying active is equally critical; incorporating consistent physical activity can aid weight management while improving overall well-being. Join community exercise groups or find postpartum fitness classes that prioritize health and healing. Taking these proactive steps can pave the way for sustained health throughout motherhood. Furthermore, educators should spread awareness about the connection between gestational diabetes and long-term health so that new mothers can take charge of their health journeys. Engaging in continuous education about nutrition and health enables informed decisions. Lastly, embrace the idea of sustainable changes, focusing on small, realistic goals to cultivate a healthier lifestyle in the long run.
Ultimately, successful navigation of postpartum nutrition following gestational diabetes rests on education, support, and commitment. There is no one-size-fits-all approach, so continuously adapting dietary needs alongside personal preferences remains vital for effective health management. Maintaining communication with healthcare professionals ensures that nutritional needs are met, addressing any concerns promptly. Registered dietitians can offer personalized meal planning sessions, allowing mothers to focus on their specific needs. Utilize resources such as online platforms and cooking classes to support healthy cooking skills. It is equally essential to maintain flexibility in dietary choices; understanding that life may get busy is vital. That said, small changes can make a significant impact over time. Establishing a routine can aid in making healthier choices more controllable and predictable. Connecting with other mothers to share tips and successes can provide mutual encouragement. Participating in community events, cooking classes, or support groups keeps motivation high and allows for social connections. Nurturing oneself while caring for a newborn is a balance; thus, integrating enjoyable nutrition practices strengthens resolve. Remember, establishing a solid foundation in postpartum nutrition not only benefits the mother but also sets the tone for a healthy family dynamic.