The Role of Abdominal Pain in Diagnosing Gut Inflammation
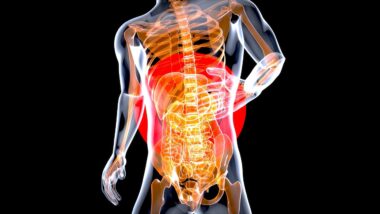
Understanding gut inflammation is essential for diagnosing various gastrointestinal disorders. Abdominal pain is often the most significant symptom that prompts individuals to seek medical attention. This discomfort can stem from several underlying gut issues, ranging from inflammation to infection. Doctors typically rely on patients’ descriptions of pain, including its intensity and location, to guide their assessment. It is vital to observe the pain’s relationship with food intake, bowel habits, and overall lifestyle, as these factors could help pinpoint the cause. Moreover, abdominal pain can present itself differently, affecting the diagnosing process. For instance, cramping suggests one type of disorder, while sharp pain indicates something potentially more acute or severe. Recognizing patterns in how and when the pain occurs can greatly assist healthcare professionals. Moreover, accompanying symptoms, such as bloating or changes in appetite, also contribute to the diagnostic process. A comprehensive approach often includes medical history, physical examinations, and potentially additional tests like imaging or lab work. By piecing together this information, healthcare providers can develop a clearer understanding of the patient’s condition, which is crucial for targeted treatment solutions.
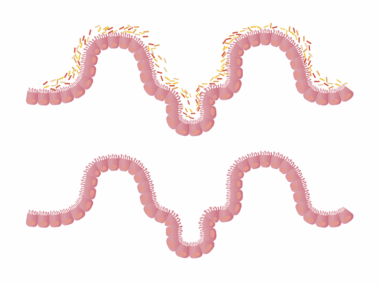
Inflammatory bowel diseases, such as Crohn’s disease and ulcerative colitis, exemplify conditions where abdominal pain is predominant. Patients often report chronic or intermittent pain coupled with diarrhea, weight loss, and fatigue. This spectrum of symptoms signifies the need for immediate medical evaluation. The diagnosing process focuses on understanding how abdominal pain fits within the wider clinical picture, facilitating an accurate diagnosis. Additionally, abdominal pain can be accompanied by other warning signs such as blood in the stool or drastic changes in bowel habits. These indications require thorough investigation, including blood tests to check for markers of inflammation and anemia. While abdominal pain is a significant symptom, it is essential to analyze it in conjunction with other signs to avoid misdiagnosis. In cases where inflammatory bowel disease is suspected, imaging techniques like MRI or CT scans may be employed for detailed examination of the gastrointestinal tract. Moreover, endoscopy can directly visualize the condition of the intestines. Early detection and diagnosis play an urgent role in preventing complications, emphasizing the importance of understanding abdominal pain and gut health. Thus, abdominal pain serves as a critical warning sign in diagnosing potential gut inflammation.
Different Types of Abdominal Pain
Abdominal pain can manifest in various forms, each pointing toward distinct underlying issues. Understanding these differences is crucial in diagnosing gut inflammation accurately. For example, localized pain, often felt on one side or in one specific area, may indicate appendicitis or diverticulitis. Conversely, generalized pain affecting multiple areas often complicates diagnosis and may suggest conditions like irritable bowel syndrome or inflammatory bowel diseases. Additionally, the nature of the pain—whether it’s sharp, dull, or throbbing—provides essential clues for healthcare professionals. Sharp, sudden pain could signify a more severe issue requiring immediate intervention. Factors like duration and timing of the pain are also informative; chronic pain may indicate a persistent underlying issue, while acute pain raises immediate concerns. Patients’ pain experiences can also vary based on factors like age, sex, and pre-existing health conditions, complicating the diagnostic landscape further. Medical professionals must consider the patient’s complete medical history along with a physical examination, allowing them to formulate a comprehensive treatment plan tailored to the individual’s specific needs. This thorough approach aids in addressing not only the pain but also the broader gut health concerns.
Besides underlying inflammation, abdominal pain can be influenced by dietary factors or external stressors. The gut-brain connection plays a vital role in how individuals perceive abdominal discomfort. Stress and anxiety can exacerbate gut symptoms, causing pain or discomfort even in the absence of a physical issue. Therefore, healthcare providers often assess patients’ mental health histories alongside their physical symptoms to identify potential connections. Furthermore, understanding how specific foods trigger or alleviate abdominal pain is essential for effective management. Individuals may benefit from keeping a food diary to help identify potential irritants and inform dietary adjustments. Common triggers include highly processed foods, dairy, gluten, and spicy dishes. By reducing or eliminating these foods, many individuals find significant relief from their symptoms. Additionally, supportive dietary approaches, such as incorporating more fiber and consuming probiotic-rich foods, can promote gut health. This holistic understanding combining both emotional and physical factors enables patients to take an active role in managing their symptoms. Thus, by addressing both the physiological and psychological aspects of abdominal pain, healthcare providers can offer more comprehensive and effective treatment strategies.
Diagnostic Tests and Abdominal Pain
To diagnose gut inflammation accurately, healthcare providers may recommend a series of diagnostic tests based on reported abdominal pain. These tests can clarify the cause of the pain and help outline a suitable treatment plan. Blood tests are commonly used to assess inflammatory markers, like C-reactive protein (CRP), and indicators of anemia. Elevated levels often corroborate clinical suspicions of an inflammatory process within the gut. Additionally, stool tests can detect pathogens, signs of inflammation, or blood, providing further diagnostic insights. Imaging studies are also crucial; ultrasound, CT scans, or MRI can visualize structural abnormalities, such as blockages or inflammation, essential in forming a diagnosis. Moreover, endoscopy and colonoscopy allow for direct visualization of the gastrointestinal tract, enabling biopsies to confirm diagnoses like Crohn’s disease or ulcerative colitis. Thus, these diagnostic strategies broaden the understanding of abdominal pain in the context of gut health. Early, accurate diagnosis is pivotal in managing inflammation, optimizing patient outcomes, and preventing complications. Without these diagnostic tests, healthcare providers may miss vital indicators that could lead to delayed treatment or misdiagnosis, emphasizing their necessity.
Upon diagnosing gut inflammation, treatment plans must be personalized to manage the specific condition effectively. Many individuals experiencing abdominal pain find relief through lifestyle adjustments, dietary changes, medication, or, in some cases, surgical interventions. For conditions like inflammatory bowel disease, medications such as corticosteroids or immunosuppressants can be effective in reducing inflammation. Additionally, medications aimed at symptom control, like antispasmodics or antidiarrheal agents, can significantly enhance patients’ quality of life. Furthermore, adopting an anti-inflammatory diet rich in omega-3 fatty acids, whole grains, and plant-based foods can assist in managing inflammation and promoting gut health. Integrative approaches, such as mindfulness practices, yoga, or therapy, can address the psychological aspects of pain and stress management, complementing physical symptom management. Regular follow-ups with healthcare professionals are essential to monitor progress and adjust treatment plans as necessary. Consequently, tackling abdominal pain and gut inflammation requires a holistic approach that combines medical treatment with lifestyle and dietary changes, enabling individuals to regain control over their health and well-being. Effective management fosters improved overall quality of life and enhances recovery, allowing individuals to pursue their daily activities without the burden of discomfort.
The Importance of Early Detection
Combating gut inflammation effectively hinges on early detection and appropriate responses to abdominal pain. Individuals who notice recurrent or persistent abdominal discomfort must seek medical advice promptly. Delays in addressing symptoms can lead to worsening conditions, making treatment more complex and challenging. Early intervention can prevent complications such as intestinal blockage, perforation, or malnutrition, significantly impacting a person’s health trajectory. Furthermore, fostering awareness about symptoms associated with gut inflammation can encourage individuals to seek help sooner. Education surrounding warning signs, such as drastic weight loss, blood in stool, or fever accompanying pain can empower patients to act decisively. Collaborative relationships between doctors and patients are critical; patients should feel comfortable discussing symptoms, concerns, and any changes in their condition. Open communication enhances diagnosis accuracy and increases the likelihood of successful treatment outcomes. Moreover, ongoing research into gut health continues to unveil new insights, underscoring the need for proactive approaches to wellness. By recognizing the importance of abdominal pain as a signaling mechanism for gut inflammation, individuals can advocate for their health more effectively. Ensuring responsive care fosters healthier outcomes and improves overall well-being.
In summary, abdominal pain serves a pivotal role in diagnosing gut inflammation. Recognizing how various types of pain correlate with distinct gut disorders can significantly impact treatment decisions and outcomes. Awareness of symptoms, accompanied by a thorough understanding of diagnostic processes, allows healthcare providers to deliver accurate diagnoses. Additionally, an integrative approach that includes dietary and lifestyle adjustments is essential for managing inflammation effectively. Patients seeking relief should be encouraged to actively participate in their care and educational outreach regarding gut health can empower individuals. Furthermore, timely detection of symptoms signals the necessity for immediate action. By understanding the intricate relationship between abdominal pain and gut health, both patients and healthcare professionals can work together to enhance diagnostic accuracy and treatment effectiveness. This collaboration fosters a comprehensive understanding which ultimately leads to better health outcomes. Prioritizing gut health is vital as it contributes to overall well-being, profoundly affecting daily life. Therefore, investing time and resources in understanding the complexities of gut inflammation is a worthwhile endeavor. A commitment to health promotion can vastly improve individual lives, encouraging a proactive approach to maintaining gut health and addressing inflammation-related concerns accordingly.