Fructose Intolerance and Digestive Health: What You Need to Know
Fructose intolerance is a condition that significantly influences digestive health and general well-being. It occurs when the body lacks the necessary enzyme to break down fructose, a simple sugar commonly found in various fruits, sweeteners, and certain vegetables. This problem can lead to several digestive challenges, including bloating, gas, abdominal pain, and diarrhea, as unabsorbed fructose ferments in the intestine. Proper recognition of fructose intolerance is crucial for anyone experiencing these symptoms, as it can help mitigate discomfort and prevent long-term health complications. The identification of fructose intolerance often involves a combination of dietary assessments and breath tests, which measure hydrogen or methane levels after ingesting fructose. Managing dietary intake is vital for individuals suffering from fructose intolerance; a low-fructose diet can alleviate symptoms and enhance the quality of life. Therefore, understanding which foods contain fructose and finding suitable alternatives is essential. It’s also important to consult a healthcare professional for a personalized plan, ensuring nutritional needs are met while avoiding trigger foods. This proactive approach assists individuals in living healthier lives despite their dietary restrictions.
Symptoms of Fructose Intolerance
The symptoms of fructose intolerance can vary widely among individuals, but they commonly manifest in gastrointestinal discomfort. Affected individuals may experience frequent bloating, cramping sensation in the stomach, flatulence, or diarrhea shortly after consuming fructose-containing foods. Some people might also feel fatigue or experience headaches linked to their dietary choices. It is crucial for those who suspect they have fructose intolerance to monitor their reactions following the ingestion of foods high in fructose. This can include popular items such as apples, pears, certain sweeteners like honey, and high-fructose corn syrup found in many processed products. If symptoms persist, consulting a healthcare provider or nutritionist might be necessary for accurate diagnosis and management. Many professionals suggest keeping a food diary to track food intake and symptoms for better insight into potential triggers and patterns. Individuals experiencing severe reactions should seek immediate medical advice, as this could indicate other underlying issues or intolerances that require attention. Recognizing these symptoms early can help in managing dietary restrictions effectively and avoiding unnecessary discomfort in daily life.
Adjusting your diet is essential for managing fructose intolerance effectively, focusing on lower fructose options. A low-fructose diet often promotes the consumption of foods that are less likely to trigger symptoms, such as certain vegetables, meat, dairy, and gluten-free grains. Foods like spinach, carrots, and potatoes are typically safe and nutritious, contributing to a more balanced diet. It is equally important to learn how to read food labels carefully, as many packaged foods contain high-fructose additives that exacerbate symptoms. Over time, individuals can identify which foods are safe and nutritious while minimizing adverse effects on their digestive health. Keeping open communication with a healthcare provider can provide valuable guidance on maintaining a well-rounded diet. Incorporating safe legumes and nuts helps diversify nutrition further. Additionally, exploring appropriate cooking methods, such as steaming or baking, can significantly enhance the digestibility of foods. Variability in individual tolerance levels necessitates personalized dietary adjustments. The goal is to maintain optimal health while enjoying a variety of foods, enhancing overall well-being for those affected by fructose intolerance.
Fructose Malabsorption vs. Fructose Intolerance
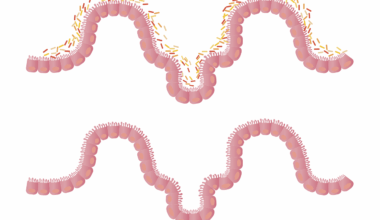
Understanding the distinction between fructose malabsorption and fructose intolerance is crucial for individuals experiencing digestive challenges. Fructose malabsorption refers to the inability to properly absorb fructose in the intestines, leading to similar symptoms but often with different underlying mechanisms. Unlike fructose intolerance, which involves a genetic condition impeding enzyme production, malabsorption typically arises from gastrointestinal issues affecting nutrient absorption. Consequently, both conditions can present identical symptoms, complicating diagnosis and management. Individuals may need to undergo specific tests to determine the root cause of their symptoms accurately. Testing may involve a breath test, which measures hydrogen levels after fructose ingestion to identify fructose malabsorption specifically. Management strategies for both conditions often overlap, generally focusing on dietary adjustments to alleviate symptoms. Nevertheless, it’s essential to approach each situation with individual considerations to address the unique challenges posed by the specific condition. Hence, receiving accurate diagnosis and tailored management strategies empowers affected individuals to navigate their dietary challenges and improve their digestive health effectively. This approach fosters a supportive environment for exploring effective coping mechanisms and health optimization.
When navigating life with fructose intolerance, awareness and education become powerful allies. Regularly educating oneself about food choices, hidden sources of fructose, and label reading enhances dietary success for individuals affected. In addition, support groups and resources can provide valuable information and emotional backing, enabling individuals to connect with others who face similar challenges. Furthermore, recipes tailored to be low in fructose can inspire creativity while maintaining compliance with dietary restrictions. Sharing experiences and tips in community settings facilitates a stronger support network for managing food intolerances effectively. Each individual’s journey can serve as motivation for others, fostering a sense of camaraderie and understanding. Moreover, self-advocacy emerges as a vital component in navigating social and dining situations where tempting foods are present. Communicating dietary needs in social settings ensures that dietary restrictions are acknowledged and respected, promoting inclusivity and safety. As awareness broadens, friends and family can learn to support loved ones dealing with fructose intolerance. Lastly, seeking guidance from registered dietitians assists individuals in crafting personalized dietary plans that prioritize health without sacrificing enjoyment or flavor in meal preparation.
Consulting a Healthcare Professional
Consulting a healthcare professional plays a pivotal role in managing fructose intolerance effectively. These professionals, including registered dietitians or gastroenterologists, can provide tailored advice based on individual needs and health conditions. An accurate diagnosis is essential for understanding the condition’s scope, ensuring dietary modifications yield beneficial results. Healthcare professionals can utilize specific assessment methods to evaluate symptoms, facilitate proper test referrals, and offer guidelines for successful dietary transitions. Additionally, ongoing support can significantly impact long-term success in managing fructose intolerance. Regular check-ups help monitor progress and adapt dietary plans as necessary, while healthcare professionals can assist in addressing emerging concerns or symptoms. Furthermore, professional insights can help navigate dining out or social situations, ensuring safe food choices under varying circumstances. Equipped with expert advice, individuals are better prepared to explore diverse food options without overwhelming fear of triggering symptoms. Continuous collaboration strengthens self-management strategies and promotes a balanced approach toward healthier dietary practices. Emphasizing professional guidance not only bolsters confidence but also encourages a deeper understanding of how to successfully adapt to life with fructose intolerance.
Research continues to advance the understanding of fructose intolerance, uncovering potential treatments and management approaches. Recent studies investigate the role of gut microbiota and its influence on fructose digestion, possibly opening new avenues for personalized treatments. Scientists focus on identifying beneficial bacteria that may enhance fructose metabolism, ultimately aiming to alleviate symptoms. Ongoing research initiatives also aim to develop effective probiotics tailored to support individuals with fructose intolerance and improve digestive health. Individuals might soon benefit from a better understanding of their condition and potential therapeutic interventions. Collaborations between healthcare professionals and researchers can foster insight into dietary interventions, leading to improved health outcomes by identifying effective strategies. Moreover, supporting policies aimed at understanding and accommodating food allergies and intolerances can create a more inclusive food environment. As the research progresses, increased awareness and education around fructose intolerance will empower individuals, simplistically breaking the stigma associated with dietary concerns. Empowering communities with knowledge can contribute to a more accommodating environment for individuals navigating daily dietary challenges, ultimately paving the way for healthier lifestyles without compromising on flavor or nutrition.