Gluten and Diabetes: Is There a Connection?
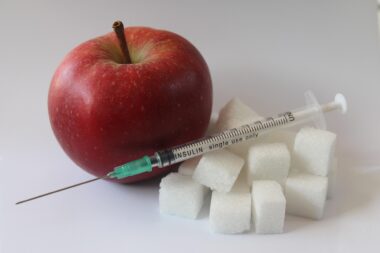
Diabetes management can be complex, requiring individuals to consider various dietary factors. One common question arising among diabetics is whether gluten plays a role in their condition. Gluten is a protein found primarily in wheat, barley, and rye. For individuals without celiac disease, gluten typically poses no threat. However, those managing diabetes must understand their dietary restrictions. Some studies suggest a link between gluten and inflammation in the body, which may affect insulin sensitivity. This could imply that some diabetics might benefit from a gluten-free diet, helping to clarify blood glucose levels. It’s important to note that simply removing gluten may not universally improve diabetes management. Consistent monitoring of blood sugar is crucial when making dietary changes. A diet rich in whole foods, fruits, and vegetables is advisable. Additionally, always consider individual responses to gluten. Consulting with a healthcare provider is recommended for personalized advice. Ultimately, identifying triggers specific to oneself will enhance overall health. As the conversation around gluten and diabetes continues, further research will help to clarify these intricate connections.
Many people with diabetes also face gluten sensitivity, a condition that can exacerbate their symptoms. Gluten sensitivity should not be confused with celiac disease, which is an autoimmune disorder. Individuals with gluten sensitivity may experience symptoms such as bloating, abdominal pain, and fatigue upon consuming gluten-containing foods. Managing these symptoms effectively can lead to better overall wellness. Diabetics who also suffer from gluten sensitivity may find that eliminating gluten from their diet results in improved energy levels and reduced gastrointestinal distress. Foods to avoid include traditional bread, pasta, and some sauces. Instead, gluten-free alternatives made from rice, corn, or quinoa can be excellent substitutes. Incorporating a variety of grains can help maintain a balanced diet while steering clear of gluten. The focus should be on nutrient-dense options. Those interested in transitioning to a gluten-free lifestyle should approach it thoughtfully. Keeping a food diary can help identify specific food triggers while allowing the tracking of blood sugar levels. Understanding individual tolerances and preferences will ultimately facilitate better health choices.
Nutritional Considerations for Diabetics
When considering gluten in the context of diabetes, it is critical to evaluate nutritional aspects. Carbohydrate content is vital for diabetics, as it directly affects blood sugar levels. Gluten-containing grains can have high carbohydrate counts. Therefore, it’s essential to focus not just on gluten presence but also on the overall nutritional value of foods. Opting for whole, unprocessed gluten-free grains provides a healthier alternative. Examples include buckwheat, millet, and gluten-free oats. These grains offer beneficial nutrients while aiding in blood sugar regulation. Additionally, incorporating proteins and healthy fats is advisable. These can help balance meals and minimize blood sugar spikes. A well-rounded meal containing vegetables, healthy fats, proteins, and gluten-free grains can support overall metabolic health. Understanding portion sizes and meal timing plays a crucial role in managing diabetes as well. Implementing these strategies can foster better glucose control over time. Ultimately, all dietary choices should align with individual health goals, preferences, and nutritional needs for optimal health outcomes.”
The relationship between gluten, diabetes, and weight management is also essential for individuals managing their health. Being overweight can exacerbate insulin resistance and worsen diabetes complications. Thus, maintaining a healthy weight is crucial. Following a gluten-free diet can sometimes contribute to weight loss, though this varies among individuals. Some gluten-free products are higher in calories and sugar, potentially hindering weight management efforts. It’s important to read nutritional labels carefully and choose whole foods over processed alternatives. Emphasizing fruits, vegetables, lean proteins, and healthy fats should remain a priority on a gluten-free meal plan. Regular physical activity is also essential in managing weight and diabetes effectively. Finding enjoyable ways to exercise can enhance adherence to routines. Many find support through community groups or online forums. These platforms can share experiences and tips related to gluten-free living and diabetes management. Accountability can make a significant difference in achieving health goals. Ultimately, finding balance and understanding your body will guide decisions that promote a healthier lifestyle.
Research and Future Implications
Ongoing research into the connection between gluten and diabetes reveals new insights continually. Understanding how gluten impacts individuals with diabetes remains complex and highly individualized. Researchers are exploring potential correlations between gluten consumption and the prevalence of type 1 diabetes, particularly focusing on early dietary interventions. There is hope that by identifying specific dietary components that may activate diabetes-related autoimmune processes, healthier prevention strategies can emerge. Additionally, studying the gut microbiome’s role in diabetes and gluten interactions could reveal further implications. A healthy gut may be linked to better blood glucose management, indicating how diet can influence gut health. Future studies will likely delve into how personalized nutrition proposals can achieve the greatest impact. Incorporating genetic differences in responses to gluten may offer promising directions for tailored dietary choices. Until definitive conclusions are reached, maintaining a proactive approach to both gluten and diabetes remains essential. Continuous monitoring, individualized meal planning, and preventative strategies can help ensure optimal health in those managing diabetes.
Community support can play a major role in managing diabetes alongside gluten considerations. Many find it helpful to connect with others facing similar challenges. Support groups, both online and offline, allow individuals to share their experiences. These communities provide a platform for sharing recipes, meal plans, and coping strategies. Finding friends or family members who are also interested in gluten-free options can promote adherence to healthier choices. Moreover, these groups can offer practical tips for dining out or navigating food markets while maintaining dietary restrictions. Engaging with nutritionists specializing in diabetes and gluten-free diets can also provide personalized guidance. Workshops and informational sessions can improve awareness of healthy food choices and preparation techniques. Making informed decisions empowered by collective knowledge will strengthen individual efforts toward better health. Networking within these communities fosters accountability and motivation, which is vital in maintaining long-term dietary changes. By sharing personal experiences, individuals can find encouragement during challenging times. Ultimately, creating a support system can enhance the management of both diabetes and gluten sensitivity.
Conclusion
In conclusion, the connection between gluten and diabetes is ongoing and multifaceted. Understanding how gluten might impact diabetes management requires navigational efforts toward tailored food choices. While some individuals may find relief through a gluten-free diet, others may not notice any changes. There’s no one-size-fits-all answer, making it crucial to prioritize individual dietary needs. Regular consultation with healthcare professionals is vital to monitor progress and adjust dietary strategies. The importance of balanced nutrition cannot be overstated—selecting whole, nutrient-dense foods should be the foundation of any dietary plan. Staying well-informed on current research can aid individuals in making educated decisions regarding their diets. Lifestyle factors such as regular exercise and stress management also contribute significantly to diabetes control. Engaging actively in the diabetes community helps bring fresh perspectives and shared insights. Personal experiences and voices are essential in shaping understanding of dietary needs. Ultimately, the journey of managing diabetes and potential gluten sensitivity involves experimentation, support, and commitment to creating a healthier lifestyle.
By embracing individual paths, exploring research, and connecting with supportive communities, individuals can navigate their unique health needs successfully. Research on gluten’s implications continues to expand, enhancing knowledge and refining strategies for effective management. Understanding personal and nutritional contexts nourishes health decisions, paving the way for improved well-being and vitality in the face of diabetes.