Exploring the Link Between Gut Microbiome and Eating Disorders
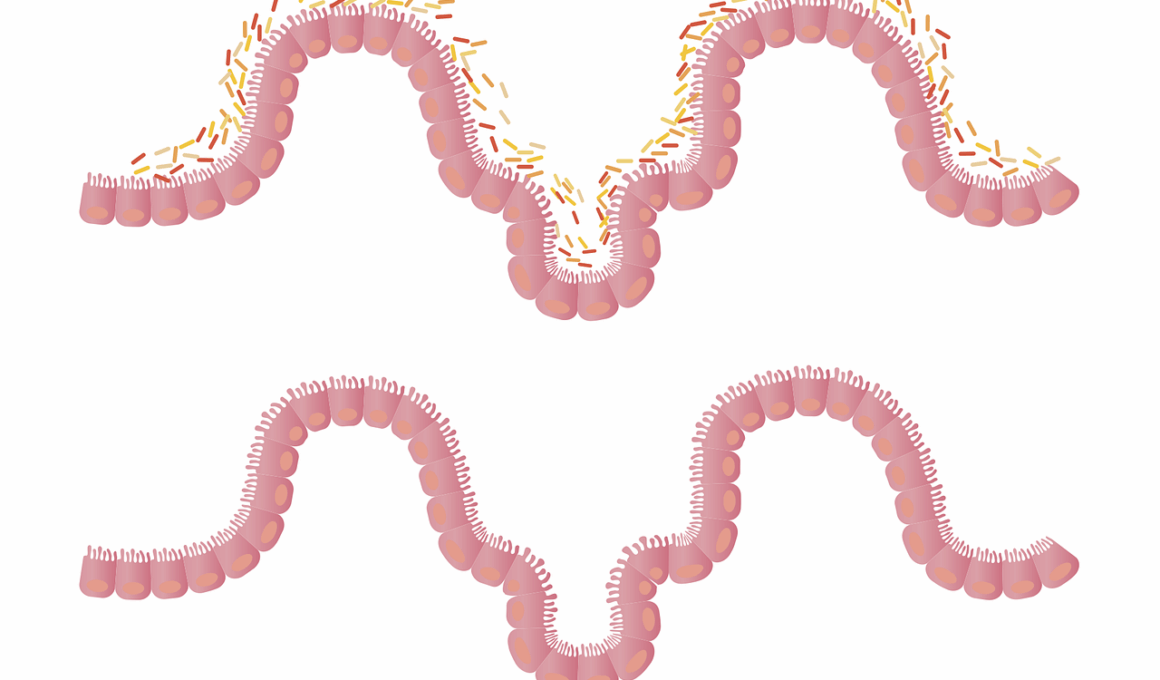
The gut microbiome plays a vital role in various aspects of health, including mental well-being. Research suggests that the gut microbiome’s composition may influence our eating behaviors and contribute to eating disorders. Disruptions in the gut microbiota can lead to metabolic dysfunctions that may increase the risk of conditions like obesity, anorexia, and bulimia. Specific strains of gut bacteria, such as Lactobacillus and Bacteroides, have been associated with body weight regulation. Maintaining balance in these bacteria is key for healthy metabolic processes. Furthermore, emotional and psychological stress can lead to changes in gut microbiota, which might perpetuate unhealthy eating behaviors. By understanding these connections, we can develop more effective strategies for treating eating disorders while focusing on restoring gut health. Integrated approaches that combine dietary interventions with microbiome-focused therapies may yield promising results for individuals struggling with eating disorders. Clinical trials exploring the effects of probiotics and prebiotics on weight management are ongoing, showing potential for new treatment options. The link between gut health and eating behaviors offers an insightful perspective into prevention and recovery strategies.
Research indicates the gut microbiome’s influence extends beyond physical health to affect emotional and psychological well-being. It’s hypothesized that the gut-brain axis plays a significant role in this relationship. The communication pathways between the gut and brain indicate that the microbiome can influence neurotransmitter production, including serotonin, often referred to as the “feel-good” hormone. This could clarify why those with disrupted gut health may experience heightened anxiety or depression, often linked to eating disorders. The bi-directional communication allows the gut to send signals to the brain, affecting mood and food choices. By improving gut health, it may be possible to positively impact emotional regulation and reduce symptoms of eating disorders. Additionally, studies show that certain dietary patterns can alter gut microbiota composition. For instance, a high-fiber diet may promote beneficial bacteria while reducing harmful strains. Interventions focusing on dietary improvements have gained attention in therapeutic settings for patients with eating disorders. Therefore, a comprehensive approach considering both nutritional intake and gut microbiome health can play a crucial role in addressing these complex issues.
The Importance of Diet in Gut Microbiome Health
Diet directly influences the composition and diversity of the gut microbiome. A varied diet rich in fiber, fruits, and vegetables supports a healthy microbial community. Conversely, diets high in processed sugars and fats can lead to dysbiosis, which is characterized by an imbalance in gut bacteria. Dysbiosis has been linked with numerous health issues, including obesity and eating disorders. Restoring microbial balance through dietary changes can be an effective strategy for weight management. Probiotics and prebiotics, two important components of a gut-friendly diet, both play essential roles in supporting gut health. Probiotics introduce beneficial bacteria, while prebiotics serve as food for these bacteria. The availability of these components in our food can be leveraged to manipulate gut microbiota positively. Consuming fermented foods, such as yogurt, kimchi, and sauerkraut, provides live probiotic cultures that can enhance gut ecology. As individuals struggling with eating disorders often exhibit unhealthy eating patterns, dietary interventions can help restore gut balance and, consequently, improve mental health. Building awareness around the importance of diet in maintaining a healthy gut microbiome is crucial.
Several studies have examined the effect of specific probiotic strains on mental health outcomes for those with eating disorders. Clinical trials have suggested that particular Lactobacillus species can significantly reduce anxiety and depressive symptoms, which correlate with improved eating behaviors. Increasing awareness regarding the impact of gut health on psychological state provides insight into new treatment avenues for those experiencing eating disorders. Furthermore, the microbiome’s role in digesting food and extracting nutrients reinforces the importance of balanced gut flora in regulating body weight. Research suggests that individuals with eating disorders often show altered gut microbiota diversity, which can affect their ability to maintain healthy body weight. By restoring gut health using tailored interventions such as diet and supplementation, it may be possible to alleviate some symptoms associated with these disorders. Future research aims to further elucidate these relationships, providing a clearer understanding of how dietary components influence gut microbiome dynamics. By adopting a holistic approach to food, mental health professionals can address not only the symptoms of eating disorders but also the underlying gut health factors contributing to these conditions.
Microbiome Testing and Personalized Nutrition
Microbiome testing is becoming an increasingly popular tool for understanding individual gut health. With advances in technology, consumers now have access to various microbiome analyses that can unveil the unique composition of their gut. This testing can identify imbalances in gut bacteria that may contribute to weight management and eating disorders. By utilizing this data, healthcare providers can develop personalized dietary plans targeted toward restoring beneficial bacteria and promoting gut health. Personalized nutrition approaches have the potential to enhance recovery from eating disorders by focusing on specific needs and preferences based on individual microbiome profiles. Furthermore, these insights allow for dietary strategies that can promote overall well-being and weight management. Customizing diets not only caters to physiological needs but also enhances compliance and sustainability in treatment regimens. As we learn more about the gut-brain connection, it becomes clear that addressing the microbiome’s intricacies through personalized nutrition may hold the key to improving mental health outcomes. Emerging research continues to support the need for individualized approaches in managing eating disorders, suggesting that every person’s journey toward healing is unique yet interconnected.
Incorporating nutrient-dense foods, probiotics, and prebiotics into the diet can pave the way for improved gut health and positive behavioral changes. Emphasizing whole foods and minimizing processed options promote the growth of supportive gut bacteria. This shift in dietary patterns not only supports microbiome diversity but also enhances overall health outcomes. Creating awareness about the importance of gut health can encourage individuals, especially those with eating disorders, to explore healthier choices that align with their wellness goals. By transforming dietary habits, it is possible to promote a favorable gut environment conducive to healing. Collaboration among nutritionists, therapists, and medical professionals will be essential in creating comprehensive treatment plans that prioritize gut health. Holistic approaches that integrate diet, emotional support, and behavioral strategies represent the future of effective treatment for eating disorders. Reframing the narrative around food and eating habits can allow individuals to view their diet as a healing tool rather than a source of distress. Ultimately, by fostering positive relationships with food, we can cultivate healthy gut microbiomes that support both physical and mental well-being.
Conclusion: The Future of Research on Gut Microbiome
The linking of gut microbiome health and eating disorders opens new avenues for research and treatment. It emphasizes the need for further studies to explore these intricate relationships in greater depth. As our understanding of the microbiome evolves, we can expect more tailored interventions and therapies aimed at restoring gut health in individuals with eating disorders. Advances in nutrigenomics, which intersect nutrition and genomics, may provide innovative solutions for personalized dietary recommendations. Further research is essential to unravel the underlying mechanisms that connect gut health and mental well-being. A multi-disciplinary approach involving nutrition, psychology, and microbiome science will enhance our capacity to address these complex issues holistically. Engaging in dialogue about the connection between gut microbiome and mental health can foster shared insights and collaborative innovations within the healthcare community. This research holds the promise of creating effective preventive and therapeutic strategies for tackling the challenges of eating disorders. With a focus on gut health, we can enhance the quality of life for numerous individuals globally while paving the way for a healthier society.
Addressing the gut microbiome’s impact on eating disorders is crucial in developing effective intervention strategies. This comprehensive viewpoint encourages exploration beyond traditional treatment paradigms. By emphasizing the importance of microbiome health, we can inspire innovative approaches to recovery that harness the gut-brain connection. Providing individuals with the tools to understand their gut health can empower them to make informed dietary choices that promote healing. As we continue to investigate the interactions between gut microbiota, mental health, and dietary habits, a clearer understanding will emerge. This knowledge can contribute to destigmatizing eating disorders and create pathways toward fostering acceptance around diverse body types and nutrition. Acknowledging the profound impact of gut health can reshape the narrative surrounding weight management and eating disorders. Engaging stakeholders in the conversation about gut microbiome health is key for driving change. As the exploration of this field grows, we can anticipate significant advancements in dietary therapies that cater to individual needs and provide much-needed support for recovery. Combining scientific expertise with anecdotal evidence from those affected can lead to a brighter future for addressing these often-overlooked health challenges.