The Effect of Metformin on Gut Microbiota and Metabolic Health
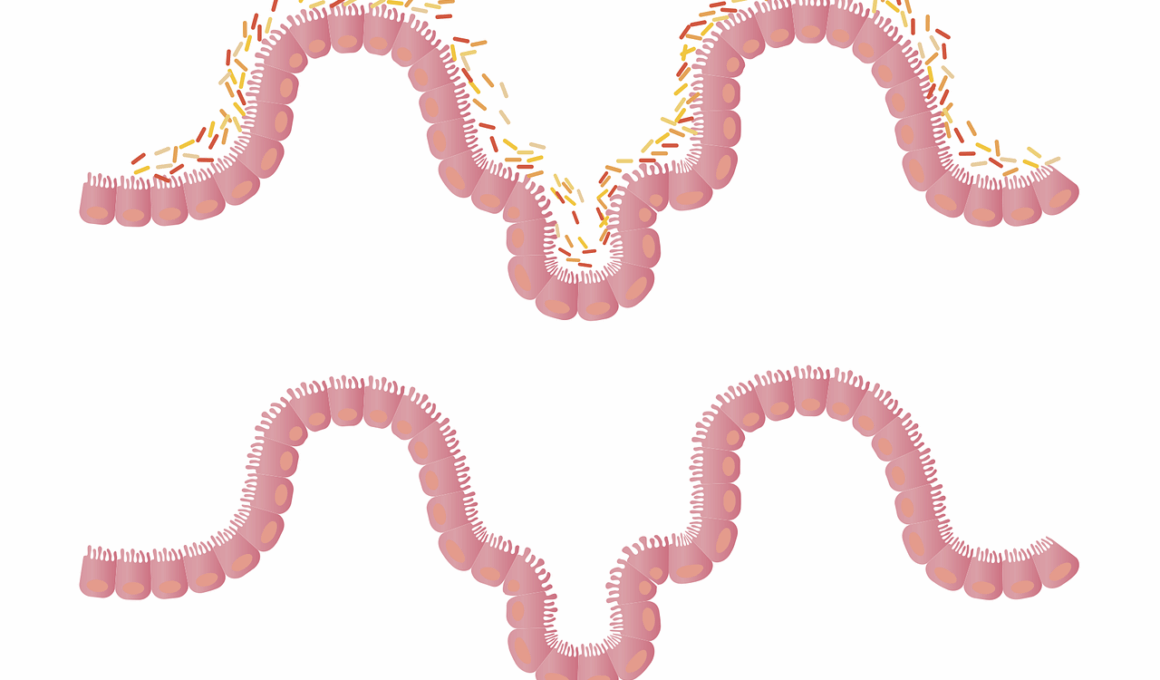
Metformin, a widely used medication for type 2 diabetes, has garnered interest for its role beyond glycemic control, specifically focusing on gut microbiota. Research reveals that Metformin significantly alters the composition of gut bacteria, influencing metabolic health. Its impact on the gut microbiome may explain some positive health outcomes associated with its use. Understanding how Metformin reshapes gut flora is crucial, as these changes can lead to improvements in insulin sensitivity, weight management, and overall gut health. More than merely a glucose-lowering agent, Metformin modifies microbial communities, promoting beneficial bacteria thought to enhance metabolic processes.
Studies conducted on patients undergoing Metformin treatment indicate a notable increase in bacterial diversity. This diversity within gut microbiota is generally associated with better metabolic health and improved resilience to disease. Some specific bacteria that flourish in response to Metformin include those from the genera Prevotella and Roseburia, which are linked to beneficial metabolic effects. Understanding these dynamics holds promise for enhancing therapeutic strategies for metabolic disorders. Furthermore, the interplay between diet and Metformin’s effects on gut bacteria may inform treatment plans, allowing healthcare providers to integrate dietary modifications alongside medication. While Metformin aids in lowering blood sugar, its potential to support gut health represents a compelling avenue for further research.
Metformin-Induced Changes in Gut Microbiota
The alteration of gut microbiota by Metformin is not merely incidental but has genuine clinical implications. As diabetic patients manage their condition, they might experience changes in their gut bacteria, promoting beneficial microbiota and reducing pathogenic types. Increased levels of short-chain fatty acids (SCFAs) are one benefit associated with this shift. SCFAs are critical for gut health and play a role in reducing inflammation and improving insulin sensitivity. Metformin’s modulation of the gut microbiome, therefore, could serve as an adjunct treatment avenue for diabetes management and associated metabolic syndromes. Continuing to explore this relationship helps elucidate how medications like Metformin carry more than just immediate therapeutic effects.
To underscore the role of a healthy gut microbiome, consider its impact on various metabolic pathways. Factors like inflammation, lipid metabolism, and insulin signaling are influenced by gut bacterial composition, which can be positively modified by Metformin use. In particular, the balance between beneficial and harmful bacteria can dictate overall health outcomes. Interestingly, Metformin may enhance the abundance of probiotic bacteria, contributing to improved gut health and metabolic function. This illustrates a holistic approach towards treating conditions like diabetes. If effectively harnessed, understanding the connection between medications and gut microorganisms could lead to more personalized and effective therapies aimed at enhancing patient quality of life.
The Interaction Between Metformin and the Gut Microbiota
Another essential element in this research involves examining how the gut microbiome interacts with other medications, affecting their efficacy. Metformin showcases how the impact of pharmacotherapy extends beyond symptom management, revealing potential synergies between gut health and metabolic control. By interacting with gut bacteria, Metformin can amplify its intended effects, optimizing diabetes treatment. Disruptions in gut microbiota can lead to adverse drug reactions, suggesting that restoring a healthy gut environment may enhance medication tolerance and effectiveness. Further examining this interplay could unveil more opportunities for developing effective treatment plans tailored to individual patient needs.
Ultimately, healthcare practitioners should remain cognizant of Metformin’s broader implications within the context of overall health, especially concerning the gut microbiome. Regular monitoring of gut health could help anticipate adjustments needed in treatment strategies for better metabolic control. Moreover, educational initiatives aimed at promoting dietary choices that complement Metformin’s microbiome benefits may empower patients. Making informed food choices that support beneficial bacteria while minimizing harmful types can harmonize treatment approaches, fostering an overall healthier lifestyle. Cultivating a healthy gut microbiome alongside conventional therapies reinforces the significance of considering individualized health strategies more broadly in diabetes care.
Conclusion: Future Directions in Research
As the connection between Metformin and gut microbiota surfaces in research, future studies should explore mechanisms of action more thoroughly. Identifying specific bacterial strains responsive to Metformin could illuminate pathways by which these agents convey systemic effects. Moving forward, clinical trials integrating gut microbiome assessments and tailored dietary interventions alongside Metformin therapy will be vital. Expanding this angle of research has the potential to reshape therapeutic guidelines, maximizing benefits while mitigating risks associated with metabolic diseases. Integrating microbiome science into diabetes treatment not only represents an exciting frontier but also emphasizes the holistic nature of health and wellness.
By advancing our understanding of medication’s impact on the gut microbiome, we stand on the brink of a new era in metabolic health care. Patients could receive tailored medication regimens that include dietary modifications, promoting bacteria that enhance the medication’s effects. Collaboration between researchers, healthcare providers, and patients can facilitate this progress, ensuring everyone shares in the benefits of gut health optimization. This approach will create numerous avenues for improved patient outcomes while transforming chronic disease management. Emphasizing the significance of a healthy gut microbiome in treatment protocols represents a pivotal shift in how medical professionals address metabolic disorders.