Dietary Patterns Associated with Improved Cognitive Outcome Post-Stroke
Stroke is a significant health issue that can lead to cognitive impairments, impacting daily living and overall quality of life. Understanding how dietary patterns influence cognitive recovery post-stroke is crucial. Recent studies suggest specific dietary approaches may support cognitive recovery. Mediterranean and DASH (Dietary Approaches to Stop Hypertension) diets are frequently mentioned as beneficial. These diets emphasize fruits, vegetables, whole grains, lean proteins, and healthy fats. Adopting these dietary patterns may reduce inflammation and oxidative stress, which are critical for brain health. Nutrient-rich foods contribute essential vitamins and minerals vital for neuroprotection. Omega-3 fatty acids from sources like fish are linked to improved cognitive function post-stroke. Polyphenols, found in berries and dark chocolate, also present protective benefits. Furthermore, maintaining appropriate hydration levels is essential for cognitive health. Effective hydration supports blood flow to the brain and enhances metabolic processes, improving brain function. As research evolves, integrating nutrition into rehabilitation is increasingly recognized as vital. Healthcare professionals should incorporate dietary counseling in recovery plans, promoting diets supportive of cognitive outcomes after a stroke.
A key consideration in dietary recovery post-stroke is the timing and customization of interventions. Individual nutritional needs can vary significantly based on factors such as age, severity of stroke, and underlying health conditions. Early and tailored nutritional interventions can enhance recovery rates and cognitive outcomes. Collaborative approaches involving dietitians, neurologists, and rehabilitation specialists ensure that dietary plans meet the specific needs of stroke survivors. Exploring patient preferences can lead to better adherence to prescribed dietary patterns, making recovery efforts more fruitful. Additionally, family involvement in meal planning can create a supportive environment for nutritious eating habits. Community resources and cooking workshops aimed at healthy eating can also empower stroke survivors. Alongside macro and micronutrient considerations, it’s crucial to address the psychological aspects of eating, improving not just physical health but mental well-being as well. Social dining experiences and group eating can facilitate a positive relationship with food, promoting both emotional and cognitive recovery. As cognitive rehabilitation progresses, ongoing assessments will help track changes in dietary habits and cognitive functions, ensuring sustained benefits from nutritional strategies.
Long-term Impacts of Dietary Patterns
Research indicates that long-term adherence to healthy dietary patterns significantly impacts cognitive outcomes post-stroke. Consistent consumption of nutrient-dense foods continues to promote neuroplasticity, allowing the brain to adapt and recover. Long-term studies show that those who maintain a Mediterranean or DASH diet exhibit slower cognitive decline than those with less healthy eating habits. The protective effects of these diets may stem from their ability to lower blood pressure and cholesterol levels, both essential for preventing further cerebrovascular events. A diet rich in fruits, vegetables, and whole grains is linked to better overall vascular health, reducing future stroke risks. Furthermore, the combination of dietary factors underlines the importance of whole-food consumption rather than isolated nutrients. The synergistic effects of these foods may enhance brain health more effectively than individual nutrients consumed separately. Integrating an array of food groups not only supports recovery but also encourages lifelong healthy eating practices. Educational initiatives aimed at informing stroke survivors about these long-term benefits can empower individuals to make informed dietary choices and incorporate healthier foods consistently.
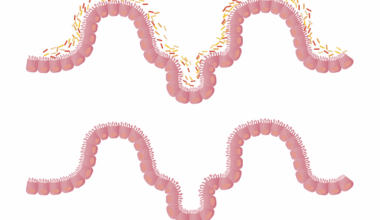
Another important aspect of dietary patterns post-stroke is the role of specific nutrients. Antioxidants, found abundantly in fruits and vegetables, contribute significantly to combat oxidative stress associated with stroke. A diet relishing antioxidants helps in minimizing cellular damage and inflammation in the brain. Nutrients like vitamins C and E and minerals such as selenium provide neuroprotective effects essential for cognitive recovery. Furthermore, B vitamins, including folate, B6, and B12, are crucial for brain function and cognitive health. These vitamins are pivotal in reducing homocysteine levels, which, if elevated, have been linked to cognitive decline. Implementing a diet rich in these vitamins can support neurological health and facilitate recovery post-stroke. Additionally, dietary fiber from whole grains and legumes promotes gut health, which is increasingly recognized for its connection to brain health. Probiotics and fermented foods can further enhance gut microbiome diversity, supporting mental well-being. Hence, a comprehensive approach that includes rich sources of these nutrients into meals is essential in forming dietary strategies beneficial for cognitive recovery after a stroke.
Challenges in Dietary Adherence
Despite the proven benefits of healthy dietary patterns, numerous challenges can affect adherence among stroke survivors. Cognitive deficits resulting from a stroke can complicate meal planning and preparation, leading to poor dietary choices. Readiness for change also varies among individuals, influenced by factors such as age, cultural practices, and socioeconomic status. Limited access to available healthy foods can hinder adherence to recommended diets, especially for those in underserved communities. Affordability is another barrier; healthier foods often come at a premium, making them less accessible. Addressing these challenges through community resources is critical. Initiatives can include establishing food banks and farmers’ markets that provide affordable healthy options specifically targeting stroke survivors. Additionally, educational programs can raise awareness about nutrition’s role in recovery. Health professionals should focus on building motivation and individual accountability, offering practical solutions that fit within each survivor’s lifestyle. Providing resources, including recipes and guided meal preparations, can simplify the transition to healthier eating. Successful outcomes rely on a well-rounded approach involving not only dietary advice but also extensive support systems tailored to individual needs.
Monitoring dietary patterns also plays a pivotal role in enhancing cognitive recovery post-stroke. Regular assessments can help identify dietary deficiencies and track adherence to the recommended eating patterns, offering timely interventions as needed. Utilizing technology can prove beneficial in tracking food intake and ensuring nutritional requirements are met. Mobile applications that promote healthy eating and provide educational materials about nutrition can motivate stroke survivors. These tools can empower individuals to be proactive about their dietary choices. Encouraging family involvement can also enhance accountability and motivate compliance with healthier meal options. Group sessions that promote shared learning can also build community support, allowing individuals to share challenges and successes in adhering to dietary recommendations. Ongoing dialogue between healthcare providers and stroke survivors is essential to adjust dietary plans based on evolving needs during recovery. The establishment of follow-up appointments can provide continuous motivation while ensuring proper monitoring of both dietary habits and cognitive outcomes. Integrating periodic reassessment into recovery plans can facilitate lasting changes and enhance cognitive recovery in the long term.
Conclusion and Future Directions
In conclusion, the role of dietary patterns in cognitive recovery post-stroke is a fascinating and evolving field of research. As evidence increasingly supports the benefits of healthy dietary approaches, it becomes paramount to incorporate nutrition into rehabilitation strategies effectively. Collaborative efforts among healthcare providers, stroke survivors, and their families are essential in fostering adherence to beneficial dietary patterns. Future research should continue exploring the relationship between specific nutrients and cognitive outcomes, aiming to establish clear guidelines for dietary interventions tailored individually and culturally. Additionally, understanding the psychological aspects of dietary changes will aid in developing comprehensive support systems. Policymakers should also address accessibility and affordability concerns, creating environments conducive to healthy eating. Meanwhile, educational efforts can empower communities to make informed choices about their diets. As the understanding of nutrition’s role in cognitive health expands, it will open new avenues for optimizing recovery strategies for stroke survivors. Ultimately, integrative approaches involving diet, physical activity, and cognitive rehabilitation can lead to improved outcomes, fostering mental resilience and well-being in patients recovering post-stroke.