Common Myths About Fiber and Chronic Illness Debunked
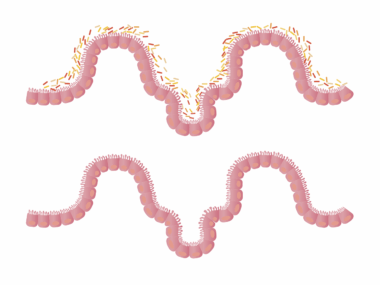
Fiber is often hailed as a health hero, especially regarding digestive health. However, myths surrounding fiber intake can mislead those with chronic illnesses. Many believe that all fiber aids digestion equally, yet this is not the case. Soluble fiber, found in oats and fruits, helps control bowel movements. In contrast, insoluble fiber may not be as beneficial for some individuals dealing with inflammatory bowel diseases. It’s essential to individualize fiber consumption based on specific health needs. Understanding these differences helps people manage symptoms better. Fiber contributes to overall gut health by promoting regular bowel movements and providing food for healthy gut bacteria. This aspect is crucial for chronic illness sufferers, as a balanced gut microbiome can influence inflammation levels. However, those unfamiliar with fiber types may unintentionally worsen their condition. Additionally, one prevalent myth is that high fiber is always beneficial, which can lead to discomfort or exacerbation of symptoms like bloating or gas. Listening to one’s body and consulting healthcare providers is vital for determining appropriate fiber levels. Unpacking these myths can empower individuals to make informed dietary choices that support their chronic health conditions.
Another common misconception is that a high-fiber diet is suitable for everyone. Many people believe they should eat as much fiber as possible without understanding their specific health conditions. For instance, individuals with certain gastrointestinal disorders may need to limit their fiber intake or gradually increase it to avoid gastrointestinal distress. Failing to differentiate between dietary needs can lead to unnecessary complications. Furthermore, another myth surrounding fiber is that its only role is digestive support. In fact, fiber has various functions within the body, including regulating blood sugar levels and cholesterol management. For people living with chronic illnesses like diabetes or heart disease, fiber plays a protective role by slowing glucose absorption and keeping cholesterol levels in check. This regulatory effect can reduce the risk of complications. Nutritionists recommend incorporating both soluble and insoluble fibers into your diet for balanced health. Foods such as beans, whole grains, and leafy greens offer combinations of these fibers. Choosing nutrient-dense sources is crucial, especially for chronic illness management, as it helps maintain overall health and wellness and allows individuals to enjoy a diverse range of foods while managing symptoms effectively.
The Importance of Gradual Fiber Increase
A frequently overlooked point is the importance of gradually increasing fiber intake. Many people mistakenly believe that eating more fiber immediately is beneficial; however, this can lead to digestive discomfort. The best approach is to increase fiber consumption slowly while monitoring how the body reacts. This strategy is especially critical for those with chronic illnesses, as sudden changes can exacerbate symptoms like bloating, cramps, or diarrhea. Start by incorporating one new high-fiber food daily and observe how your body responds. Along with food introduction, it’s essential to drink plenty of water to aid the digestive process while increasing fiber. Staying hydrated ensures that fiber can perform its job effectively by helping to form stool and prevent constipation. If discomfort occurs, it’s advisable to consult a healthcare professional before making further dietary changes. This tailored approach empowers individuals to monitor their digestive health while adapting their diets. The goal should involve a sustainable fiber increase rather than a quick fix. By taking these small steps, people can achieve the overall benefits of fiber without suffering from distressing symptoms. Careful management of fiber can vastly improve quality of life for those with chronic conditions.
Moreover, a widespread myth regarding fiber is that it solely comes from plant-based foods. While it’s true that fruits, vegetables, whole grains, and legumes are excellent sources, animal-generated compounds are also rich in nutrients supporting gut health. For instance, certain dairy products like yogurt can promote a healthy gut and contribute to maintaining overall health. Probiotic-rich foods play a role in gut microbiome balance and can help treat or alleviate chronic illness symptoms. Hence, it is crucial not to discount diverse food sources that can complement a fiber-rich diet. In particular, individuals with lactose intolerance or those on a vegan diet must explore alternative options. Fortified foods and supplements may provide fiber and probiotics as invaluable allies in chronic disease management. Additionally, including prebiotic foods such as garlic, onions, and asparagus supports beneficial gut bacteria growth. By embracing varied food sources, individuals can create a well-rounded diet that meets their health goals. Keeping an open mind towards food inclusivity ensures balanced nutrition, essential for managing chronic health conditions effectively. Ultimately, viewing fiber within the broader dietary context enables individuals to harness the full benefits for their health and wellbeing.
Reading Food Labels for Better Choices
Another important aspect of fiber management in diet pertains to reading food labels. There’s a prevalent myth that all processed foods are low in fiber. However, many packaged foods can provide a good amount of fiber if chosen wisely. Carefully checking nutrition labels can guide consumers in selecting options that are nutritious alternatives. Look for cereals, bread, and snacks explicitly labeled as high in fiber. Understanding that not all fiber is created equal is essential, as some processed foods contain added fiber, which may not provide the same benefits as whole foods. Always consider ingredients and overall nutritional value when selecting food products. The fiber content can significantly vary, requiring educated decisions for health optimization. It’s also worth noting that some advertisements may exaggerate fiber content; hence, cross-referencing with reliability metrics can prove beneficial. Additionally, familiarizing oneself with various fiber types can also help when seeking out the best products. By becoming discernible label readers, individuals can better navigate choices tailored to their health needs and preferences. By adopting this habit, everyone can embrace a fiber-rich diet that effectively supports chronic illness management, thus enhancing overall well-being.
Finally, understanding the connection between fiber, diet, and chronic illness nuances is vital. Many individuals hold the belief that simply consuming fiber can resolve chronic health issues, although this is a simplification. Chronic conditions often require a multi-faceted approach encompassing diet, lifestyle, and medical interventions. No single nutrient can serve as a magic bullet for health challenges; dietary choices should involve intentional planning. Instead, fiber should be viewed as one element of a diverse nutrition plan. It’s critical to collaborate with healthcare professionals to create personalized nutrition plans. This collaboration can aid in isolating any foods that may trigger adverse reactions or precisely tailor fiber types that work best for specific conditions. Chronic illness management also relies on moderate physical activity to foster a balanced lifestyle. Incorporating movement alongside a fiber-rich diet can enhance digestion and overall health. Therefore, awareness of varying essentials within the diet is key for individuals seeking improvements in their well-being. Taking a holistic perspective on health enables a comprehensive understanding of how all factors intertwine for effective management.
Conclusion: Empowering Yourself with Knowledge
In conclusion, debunking myths regarding fiber intake empowers individuals with chronic illnesses to make informed decisions that positively affect health. By understanding fiber types, focusing on personalization and consultation with health professionals, and considering food labels, individuals can navigate dietary choices more effectively. The journey toward managing chronic illness requires persistence and education, emphasizing the importance of fiber. The ultimate goal is to encourage balanced, nutrient-rich diets conducive to better health outcomes. These choices profoundly influence the quality of life for chronic health sufferers. Additionally, individuals can seek support from communities, online forums, or programs specializing in chronic illness management for further assistance. Connecting with others in similar situations often provides motivation and inspiration. From cooking together and sharing recipes to understanding the latest research on nutrition and chronic health, these interactions can deepen knowledge and foster resilience. Knowledge is power, enabling individuals to advocate for their well-being and make decisions that enhance life quality. Armed with accurate information and understanding, we can cultivate healthier, vita-fortifying diets tailored to individual needs. This proactive approach ultimately leads to improved health outcomes and a more balanced life amidst chronic illness challenges.
Moreover, staying educated about ongoing research in dietary fiber and chronic illness is essential for ongoing health management. Dietary guidelines evolve; thus, continued learning about nutrition ensures that the information one acts upon remains current and valid. Embracing new findings fosters an adaptive mind, allowing dietary adjustments that reflect emerging knowledge. Engaging with local health workshops, nutrition seminars, or participating in online health courses can be excellent avenues for acquiring new insights. This commitment to learning underscores the proactive approach every individual fighting chronic illness should adopt for better health outcomes. Collaboration among healthcare providers must remain strong, with professionals continuously updating patients on relevant studies and findings. Additionally, advocating for further research in this area can enhance our understanding of complexities surrounding fiber and chronic disease. This collective effort helps create a more comprehensive framework for addressing chronic health issues through nutrition. In doing so, an empowered community can drive positive changes toward healthful practices. Ultimately, our relationship with food can evolve, aligning with advancing knowledge; this evolution creates the chance to transform chronic illness management effectively.