Comparing Gut Microbiome Profiles of Autistic and Neurotypical Individuals
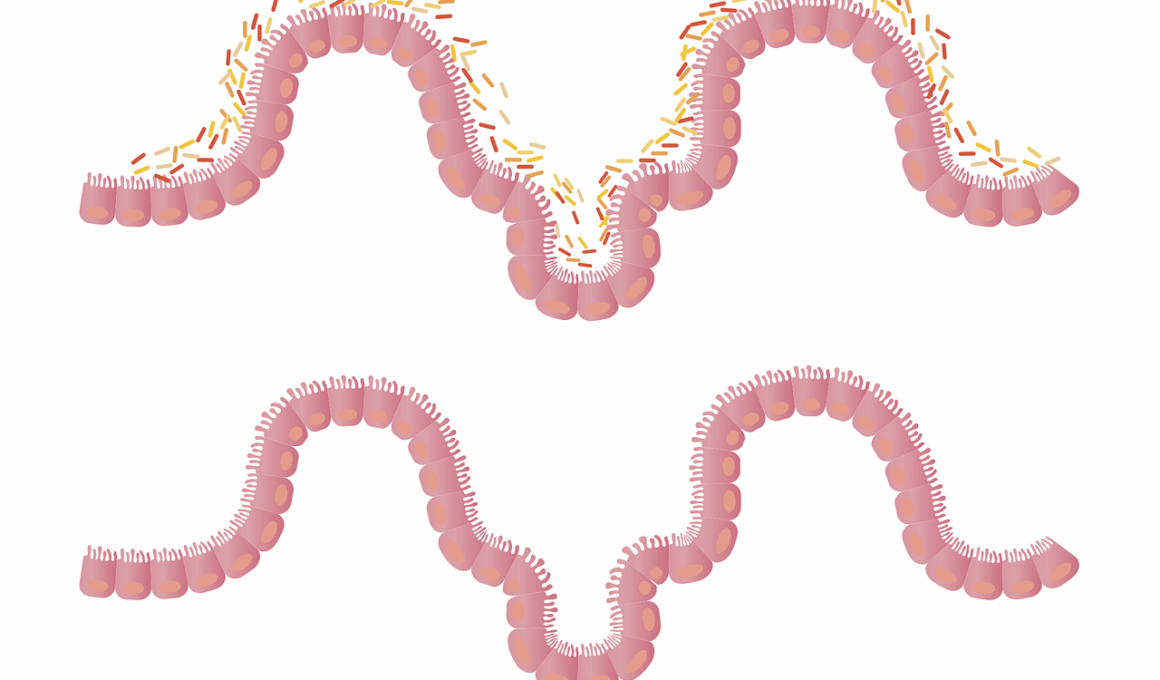
The gut microbiome plays a significant role in human health and has been increasingly studied for its potential link to various disorders, including autism spectrum disorder (ASD). Research indicates that the composition of gut bacteria differs between autistic individuals and neurotypical individuals. In many studies, it has been noted that children with autism often have dysbiosis, a condition characterized by an imbalance in the microbial communities. This imbalance may influence metabolic processes, immune response, and even neurological functions. Specific bacterial taxa, such as Prevotella and Bacteroides, have been found to be in altered proportions in autistic children compared to their neurotypical peers. Furthermore, the gut-brain axis mechanisms suggest that these microbiotic differences could affect mental health and behavioral patterns. The evidence is accumulating to support the theory that a healthier, balanced gut microbiome may contribute to improved behavioral outcomes in individuals with ASD. Future research is crucial to explore how gut-based therapies might alleviate symptoms and enhance the quality of life for those affected by autism.
Key Findings from Microbiome Studies
Several studies have shown clear differences in the gut microbiota of autistic individuals when compared to neurotypical controls. Notably, researchers have observed decreased diversity in the gut microbiomes of autistic individuals. This lack of diversity can lead to poor metabolic outcomes and has implications for cognitive development. Key bacteria types are often underrepresented, impacting the overall balance needed for optimal health. For instance, levels of beneficial bacteria like Bifidobacterium may be lower, which could influence gut health and immune functions. Additionally, elevated levels of certain inflammatory bacteria have been linked with autism symptoms. These findings highlight the potential role of dysbiosis in the manifestation of ASD symptoms. Another interesting aspect is the correlation between gut microbiome composition and gastrointestinal complaints often reported by autistic individuals. Addressing these microbiomic alterations through dietary and probiotic interventions may provide a pathway to better health outcomes and symptom management.
One promising area of research involves probiotic supplementation as a means to restore healthy gut microbiota in individuals with autism. Some studies indicate that introducing specific strains of probiotics can help rebalance the microbiome, promoting growth of beneficial bacteria while inhibiting the harmful ones. As a result, autistic individuals could experience reduced gastrointestinal discomfort, which has been increasingly linked to behavioral issues. Moreover, this emerging therapeutic strategy suggests the possibility of creating customized probiotic formulas tailored to individual microbiome profiles. Assessing personal microbiome data could lead to personalized treatment approaches, enhancing the effectiveness of interventions. Furthermore, dietary changes such as increasing fiber intake and reducing processed foods could also support microbiome health. Implementing these changes may not only influence gut health but also impact overall well-being. Ongoing clinical trials are focusing on the connection between dietary patterns and gut microbiome restoration, aiming to unearth additional benefits that could positively affect autistic individuals’ quality of life.
Gut Microbiome and Neurodevelopment
The relationship between the gut microbiome and neurodevelopment is a burgeoning field of study. Current research suggests that gut bacteria may impact the development of neural pathways during critical periods in childhood. By influencing gut health, we may also be altering how the brain processes information and responds to the external environment. The gut microbiome’s metabolites, such as short-chain fatty acids, play a significant role in brain health and behavior. The production of neurotransmitters like serotonin also occurs in the gut, raising questions about the microbiome’s influence on mood regulation and anxiety, common comorbidities in autism. Understanding this connection may provide insights into the underlying biological mechanisms that contribute to ASD. By exploring how gut-microbiome alterations correlate with neurodevelopmental outcomes, researchers hope to identify ways to support individuals with autism more effectively. This evolving understanding indicates that interventions targeting gut health may offer additional benefits within the broader spectrum of autism therapy.
There is growing interest in exploring dietary interventions as a means to modify gut microbiome composition. Recent findings indicate that a diet rich in fruits, vegetables, and whole grains can promote a healthier microbiome, which may play a role in improving symptoms associated with autism. Additionally, avoiding certain food additives and sugars has been suggested to reduce gut inflammation and microbial imbalances. Specific diets, like gluten-free and casein-free (GFCF), are gaining attention among parents for their positive anecdotal reports; however, scientific evidence remains limited. Advocating for further, rigorously controlled studies is essential to validate the efficacy of dietary changes in influencing microbiome profiles. Understanding these dietary impacts on gut health can inform parents and caregivers about potential benefits. Educating families about the significance of gut health also encourages a more proactive approach to managing autism symptoms. Ultimately, continued research into dietary modification could unlock more tools for practitioners in the fight against ASD.
Future Perspectives
Looking forward, the integration of microbiome analysis into autism research provides a rich landscape for future explorations. Investigating the role of environmental factors and their influence on the microbiome can help clarify the roots of autism. Researchers are beginning to understand that genetic predispositions for autism might interact with microbiome profiles, leading to unique developmental trajectories. Continued advances in microbiome sequencing technologies and data analysis will allow for more comprehensive insights. Furthermore, collaboration between fields such as psychiatry, nutrition, and microbiology will be essential in forming a unified approach. It is hoped that holistic intervention programs, combining diet, probiotics, and behavioral therapies, could significantly improve outcomes for autistic individuals. These comprehensive strategies are not merely about altering gut health; they also seek to create an integrated approach to autism management. Future breakthroughs could result in novel therapies, offering promising avenues for those navigating the complexities of autism.
In summary, the gut microbiome presents a fascinating arena of study in understanding autism spectrum disorder. The differences observed in gut microbiome profiles between autistic and neurotypical individuals highlight a compelling area for further investigation. Continued exploration is crucial to uncover the biological underpinnings that link gut health with behavioral and cognitive outcomes in autism. By addressing gut imbalances and promoting healthier microbiomes, there is potential for new therapeutic interventions that can help improve the quality of life for those affected. It is vital for ongoing research to remain a priority, as our understanding of the gut-brain connection continues to evolve. As science progresses, the hope is to bridge the gap between microbiome health and neurodevelopmental functioning to create supportive solutions. The journey to better outcomes for individuals with autism necessitates a multi-faceted approach, merging medical, psychological, and nutritional insights into a cohesive treatment strategy.
Ultimately, increased awareness about the microbiome’s role in autism opens the door to new possibilities for intervention. The potential for dietary modifications, supplemented by probiotics and medical support, may provide much-needed relief for families experiencing the challenges associated with autism. The pursuit of understanding the intricate relationship between gut health and brain functioning could reshape interventions significantly. Clinical guidelines may evolve to encompass gut health, offering families a more comprehensive toolkit for managing autism. The convergence of emerging research findings with lived experiences may drive better support systems. As communities embrace the notion of gut health’s impact on mental health and cognitive function, it emphasizes the necessity for holistic healthcare approaches. Future studies must strive to translate research into practical applications, ensuring that advancements benefit everyone affected by autism. Through education, awareness, and scientific exploration, we stand on the cusp of potentially transformative solutions that empower individuals with autism and their families.