Developing a Support Plan for Chronic Gut Conditions
Chronic gut conditions can significantly impact an individual’s quality of life, prompting the need for a comprehensive support plan. To ensure proper management, consider assembling a multidisciplinary team comprised of healthcare professionals. This team might include a gastroenterologist, dietitian, psychologist, and possibly a physical therapist as they work on your recovery. Each professional can offer unique insights into how to better manage your symptoms. Furthermore, they can create an integrated care plan that supports your physical and mental health. Education is vital, so it’s recommended to participate in workshops or support groups related to gut health. These resources may provide emotional support and information on lifestyle changes. Additionally, it’s crucial to monitor your condition’s progression and adapt your plan as needed. Keeping a food and symptom diary can help identify potential triggers and dietary needs. Effective communication with your team about your experiences will aid in adjusting the support plan over time. Adequate support from family and friends is also essential, encouraging adherence to recommended therapies and making necessary lifestyle modifications.
Meal planning is a critical component when managing chronic gut conditions. Women and men alike can benefit from having a well-structured diet that emphasizes a balance of macronutrients and micronutrients. Certain foods may be beneficial for gut health, while others could worsen symptoms. A well-functioning digestive system often thrives on fiber-rich fruits, vegetables, and whole grains, so incorporating these foods can be advantageous. On the contrary, foods high in sugar, unhealthy fats, or artificial additives may exacerbate gut issues. Maintaining a journal can provide an invaluable resource for tracking food choices and their effects on your wellbeing. Seek assistance from a registered dietitian in crafting a personalized meal plan focused on gut healing. They can suggest recipes, substitute ingredients, and help in finding suitable food options. Additionally, staying hydrated is paramount; drinking sufficient fluids daily can facilitate digestion and nutrient absorption. Explore options such as herbal teas or infused water for variety. You might consider avoiding strict diets that eliminate entire food groups unless advised, as they can lead to nutritional deficiencies.
Emotional and Mental Health Considerations
Chronic gut conditions can impose emotional and psychological challenges, making mental health support equally important in developing a support plan. Stress and anxiety can affect digestion, leading to a vicious cycle of worsening symptoms and emotional distress. Consider therapy options such as cognitive-behavioral therapy (CBT) or mindfulness practices that may help improve mental well-being. Engaging in stress-reducing activities like yoga, meditation, or deep breathing exercises provides effective tools for managing symptoms. Connecting with online forums or local support groups can offer community support and shared experiences, fostering resilience and coping strategies. Journaling may also be a helpful practice to process emotions surrounding chronic health conditions. Be open to discussing your feelings with friends or family members as they can provide emotional support. Balanced nutrition and regular physical activity can contribute positively to both physical and mental health. Seeking out relaxation techniques allows individuals to foster a sense of control over their symptoms. It’s vital to remember that emotional health plays a significant role in overall gut health and should not be overlooked.
Regular physical activity should be integrated into your support plan for chronic gut conditions. Moderate exercise can improve gut motility, strengthen muscles, and reduce symptoms of certain gastrointestinal disorders. Begin with activities suited to your physical capabilities, like walking, swimming, or biking. It’s essential to listen to your body and avoid overexertion, which may lead to adverse effects. Research shows that consistency is more impactful than intensity; aim for at least 30 minutes of moderate activity most days of the week. However, consult with your healthcare team before starting any new exercise regimen, especially if you have other health concerns. Incorporating stretching and flexibility exercises can help with physical comfort. Additionally, consider participating in gentle activities such as Pilates or tai chi, as these may improve overall well-being. You’ll likely find that small changes in routine can lead to substantial benefits for your gut health. Keeping track of your progress can be motivating. Establishing exercise buddies may help maintain accountability and improve social connections while making your routine more enjoyable.
Using Supplements Wisely
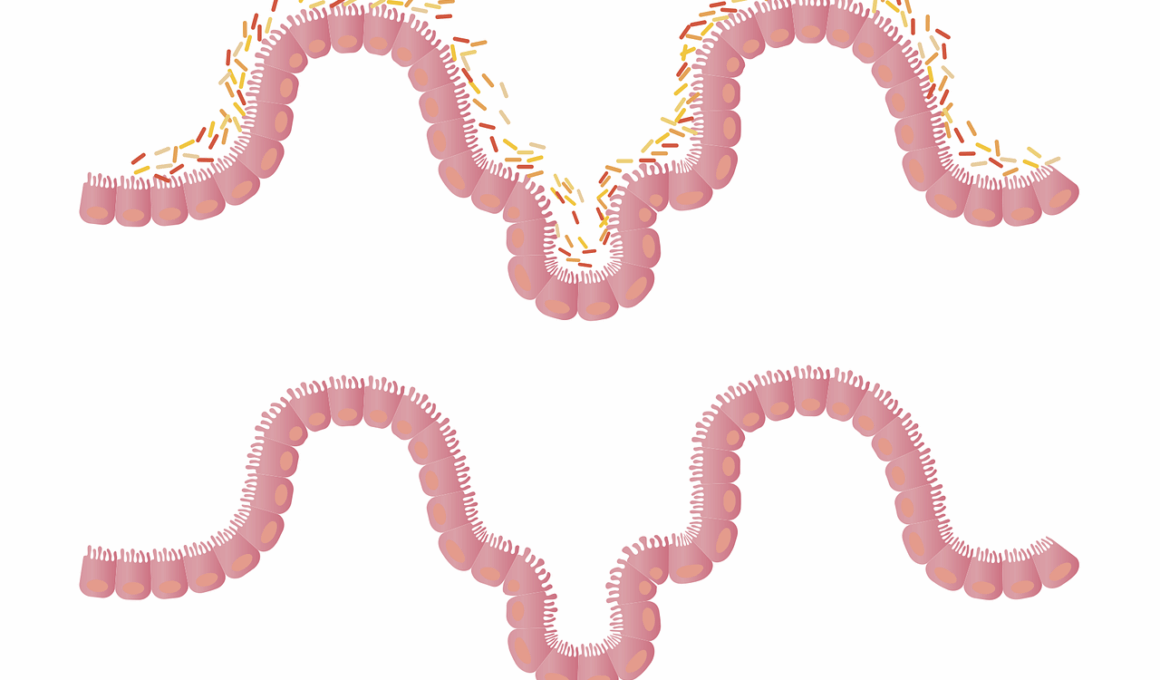
Including supplements in your support plan can be beneficial, but they should be approached cautiously and under professional guidance. Probiotics are a popular option; these good bacteria can help restore gut flora balance and support digestion. However, choosing the right strain is crucial, as different probiotics target various health issues. You might also research other supplements like prebiotics, digestive enzymes, and certain vitamins or minerals to support gut health. Always discuss any supplements with your healthcare team to avoid interactions or unwanted side effects. It’s essential to prioritize whole foods for nutrient intake before considering supplements. Some supplements may effectively address specific deficiencies or gut issues but should be viewed as adjuncts to a balanced diet. Lifestyle habits such as sleep hygiene, stress management, and regular meals can have more immediate impacts on your well-being. Therefore, supplements should not replace a well-rounded diet. While supplements can be helpful, it’s advisable to monitor their effects on your body and adjust accordingly under guidance from your healthcare team.
Ensuring social support is essential when managing chronic gut conditions. A strong network of family and friends can play a vital role in your healing process, providing emotional reassurance and motivation. They can assist by helping prepare meals, participating in physical activities, or even just listening to your concerns. Consider openly discussing your condition with loved ones, making them aware of your needs and challenges. Engaging with community resources, such as support groups or online forums, can create a sense of belonging and insight from others facing similar problems. These interactions allow for sharing effective strategies and practical tips. Foster genuine connections with those who understand the reality of chronic fasting conditions; experiences and coping mechanisms shared can significantly lighten emotional burdens. Additionally, maintaining open lines of communication with your healthcare providers aids in achieving positive outcomes, as they can tailor solutions based on your feedback. Prioritize self-care, which can manifest in various ways, including pursuing hobbies and interests that bring joy. Striking a balance between personal time, social interaction, and health management can greatly enhance your overall well-being.
Monitoring and Adjusting Your Plan
Finally, regularly monitoring your progress and adjusting your support plan for chronic gut conditions is vital in ensuring continued success. Set specific, measurable goals to help assess your progress over time. Regularly review both your symptom diary and meal logs to recognize trends and potential triggers. Staying flexible is essential; what works initially may need alterations as your condition evolves. Do not hesitate to consult with your healthcare team regarding any concerns or questions about your current approach. Utilizing regular check-ups can help you adjust your strategies, ensuring that you are on the right path to managing your gut health effectively. You may find it helpful to create a schedule for reviewing your plan, keeping your treatment on track. This allows for maintaining open communication with your healthcare team and enables you to initiate conversations about any necessary changes. A support plan should be dynamic, reflecting your lifestyle and health changes. Personal commitment to your health journey will often yield positive results in managing chronic gut conditions as you remain patient and persistent.
Conclusion
In conclusion, developing a comprehensive support plan for chronic gut conditions involves various aspects of health management focusing on individual needs. Through collaboration with professionals and support networks, you can work toward a balanced regimen that promotes gut health. Employ strategies in meal planning, exercise, and mental well-being. Maintaining open communication with healthcare providers contributes significantly to effective care. Remember that achieving wellness takes time and requires patience. Monitoring symptoms and adjusting plans plays an integral role in success. With a supportive environment in place, addressing chronic gut issues can become an attainable goal. Make sure to celebrate the small victories along the way, building resilience against challenges. By prioritizing gut health and implementing a cohesive plan, you can work towards a healthier, happier life. Stay committed to your journey and take proactive steps in living with your unique needs. Everyone can achieve a better quality of life with the proper strategies tailored to their situation. Ultimately, each aspect of your support plan contributes to a more holistic approach to gut health, allowing for meaningful advances in overall well-being.