How Gut Microbiota Influences Metabolic Inflammation
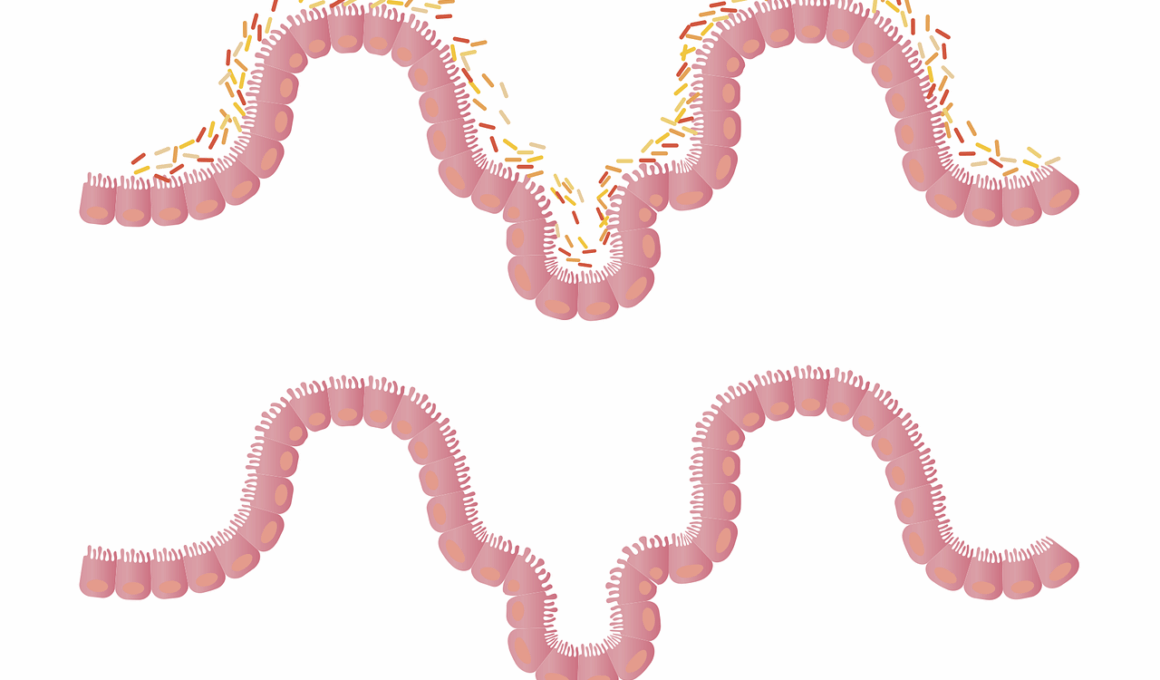
The gut microbiome plays a crucial role in regulating our metabolism and overall health. It consists of trillions of microorganisms, including bacteria, viruses, and fungi, residing in our intestinal tract. This complex community influences digestive processes, nutrient absorption, and immune response. An imbalance in gut microbiota can lead to metabolic disorders, contributing to inflammation and various health consequences. Metabolic inflammation is associated with conditions such as obesity, diabetes, and cardiovascular diseases. The interactions between gut microbiota and the host’s metabolism occur through several mechanisms. These include the production of short-chain fatty acids (SCFAs), modulation of the gut barrier function, and signaling to immune cells. Healthy gut bacteria can produce SCFAs, which reduce inflammation and promote insulin sensitivity. In contrast, dysbiosis, or an imbalance of gut microbes, can trigger pro-inflammatory pathways. This highlights the need for personalized dietary strategies aimed at fostering a healthy microbiome. By understanding the relationship between gut health and metabolic inflammation, healthcare providers can develop preventive measures and treatments tailored to individual microbiome profiles.
In understanding the impact of gut microbiota on metabolic inflammation, it is essential to explore diet’s role in shaping gut health. Dietary choices can significantly influence the composition of gut microbiota. Foods rich in fiber, polyphenols, and fermentable carbohydrates are beneficial for promoting diversity among gut bacteria. High-fiber foods, such as fruits, vegetables, and whole grains, support the growth of health-promoting bacteria, which in turn can help mitigate inflammation. Additionally, fermented foods like yogurt and kefir contain probiotics that can directly enhance the gut microbiota. On the other hand, diets high in sugar, unhealthy fats, and artificial additives may lead to dysbiosis. This imbalance can exacerbate inflammatory responses, promoting the onset of metabolic diseases. Identifying food patterns that foster a healthy gut microbiome is vital for safeguarding metabolic health. Ongoing research suggests that the Mediterranean diet may offer protective benefits due to its emphasis on whole foods and anti-inflammatory properties. Therefore, optimizing gut microbiota through dietary interventions could be a promising strategy to promote metabolic health and prevent inflammation.
Emerging evidence suggests that gut microbiota influences metabolic inflammation not only through dietary mechanisms but also through other lifestyle factors. Regular physical activity, for instance, is known to positively affect gut microbial diversity. Exercise promotes an increase in beneficial bacteria, which can enhance metabolic health and reduce systemic inflammation. Conversely, sedentary lifestyles may contribute to dysbiosis and subsequent inflammation. Additionally, other lifestyle factors, such as sleep quality and stress management, are essential for maintaining a healthy gut microbiome. Poor sleep patterns can negatively impact the composition of gut bacteria, while chronic stress is associated with gut permeability issues, leading to increased inflammation. Understanding how these lifestyle components interact with gut health provides valuable insights for preventive health strategies. Implementing a holistic approach that incorporates healthy eating, regular physical activity, and stress management can significantly influence the state of the gut microbiota. It highlights the potential for gut microbiota-centered interventions in addressing metabolic inflammation and enhancing overall well-being. Furthermore, future research must include the exploration of various lifestyle interventions that may yield positive outcomes.
The Role of Probiotics in Metabolic Health
Probiotics are live microorganisms that offer health benefits when consumed in adequate amounts. They are well-documented for their role in gut health but also show potential in managing metabolic inflammation. Clinical studies have begun to delineate how probiotics can help restore balance in gut microbiota, particularly in those suffering from obesity or type 2 diabetes. These beneficial microbes can produce SCFAs and other metabolites that have anti-inflammatory effects. Additionally, probiotics may enhance insulin sensitivity and lower blood glucose levels. This suggests that incorporating specific probiotic strains into diets may offer a therapeutic avenue for improving metabolic conditions. Fermented foods rich in probiotics, such as kimchi, sauerkraut, and yogurt, can support gut health while providing essential nutrients. Ongoing research is focusing on identifying which strains are most effective for metabolic health. Individual responses to probiotics can vary, making personalized approaches critical for optimizing interventions. A tailored microbiome profile can help determine the most beneficial probiotics suited to each individual’s metabolic condition. Overall, the integration of probiotics into diets holds promise for bolstering metabolic health and combating inflammation.
In addition to probiotics, prebiotics play a critical role in shaping the gut microbiome and influencing metabolic inflammation. Prebiotics are non-digestible fibers that serve as food for beneficial gut bacteria. They help drive the growth and activity of these microorganisms, ultimately supporting a balanced microbiome. Foods rich in prebiotics include garlic, onions, asparagus, and bananas. By enhancing the growth of beneficial bacteria, prebiotics can contribute to increased SCFA production, which has anti-inflammatory effects. The synergistic relationship between prebiotics and probiotics creates a favorable environment for beneficial microbial populations, further promoting gut health and metabolic function. A diet that emphasizes both prebiotics and probiotics may offer the best outcomes for preventing metabolic inflammation. Additionally, research indicates that specific prebiotic fibers may modulate the immune system, leading to reduced inflammation. Understanding the interplay between prebiotics, probiotics, and metabolic health can guide dietary recommendations and supplementation strategies aimed at reducing inflammation. As dietary patterns evolve, a focus on maximizing prebiotic and probiotic intake may provide a holistic approach to improving gut microbiota health and, subsequently, metabolic outcomes.
While the influence of gut microbiota on metabolic inflammation is well-established, further research is essential for understanding the underlying mechanisms. Ongoing studies are investigating the pathways through which gut microbes communicate with the host’s immune system. For instance, recognition of specific microbial components by immune cells can trigger inflammatory cascades or promote regulatory responses. This dual role highlights the complexity of the gut-immune axis and its significance in metabolic health. Furthermore, understanding genetic predispositions that affect individual microbiome composition can help tailor interventions. The interplay between genetics, environment, and gut microbiota offers a multifactorial perspective on metabolic inflammation. Integrative approaches that consider genetics, lifestyle factors, diet, and microbiome composition will be paramount in developing personalized healthcare strategies. Additionally, researchers are exploring novel therapeutic avenues, such as microbiome modulation through fecal microbiota transplantation, which may hold promise in treating metabolic conditions. Collaborative efforts among researchers, healthcare practitioners, and patients will be essential in translating findings into actionable interventions. Continuous exploration into this field will pave the way for innovative therapies aimed at improving gut health and mitigating inflammation.
The emerging relationship between gut microbiota and metabolic inflammation emphasizes the importance of a healthy lifestyle. Active awareness of dietary habits, exercise routines, and stress management is essential in promoting optimal gut health. Community education and outreach programs play a vital role in informing the public about the significance of microbiota in metabolism and health. Creating a greater awareness of how food choices, physical activity, and overall wellness affect gut health will empower individuals to make informed decisions. As scientific evidence continues to unfold, the integration of microbiota-centered approaches into public health initiatives will be necessary. Moreover, collaboration with healthcare professionals can ensure the application of such strategies in clinical settings. Additionally, personalized nutrition may soon become a cornerstone of dietary recommendations, focusing on individual microbiome profiles for tailored interventions. By prioritizing gut health through multifaceted approaches, society can work towards preventing metabolic inflammation and its associated diseases. Ultimately, a well-informed public that understands the critical role of gut microbiota will foster healthier communities and improve metabolic outcomes at large.