Heartburn and GERD: Tips for Effective Management
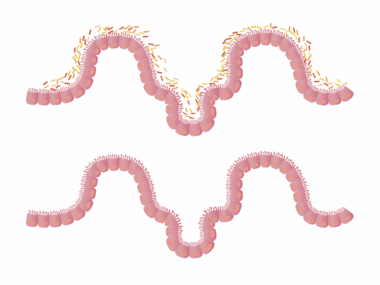
Heartburn and gastroesophageal reflux disease (GERD) are common gut disorders affecting millions of people worldwide. Both conditions arise from the backward flow of stomach acid into the esophagus, leading to discomfort and complications. To effectively manage these issues, it is essential to understand their symptoms and root causes. Heartburn presents as a burning sensation in the chest, usually after eating, while GERD may include additional symptoms like chronic cough and difficulty swallowing. Lifestyle modifications are crucial in managing these conditions. Many find relief by making specific dietary changes, such as avoiding spicy foods, citrus fruits, and carbonated beverages. Additionally, maintaining a healthy weight can greatly reduce the risk of acid reflux. Elevating the head of the bed and avoiding lying down after meals are other practical strategies. In some cases, medical intervention may be necessary, including over-the-counter antacids or prescription medications. Always consult a healthcare professional for personalized treatment options. By keeping a food diary and noting triggers, individuals can better manage their symptoms and prevent flare-ups. Identifying personal triggers is key to effective management.
It’s important to recognize the distinction between heartburn and GERD. Heartburn is often an occasional inconvenience, while GERD is a chronic condition requiring ongoing management. Understanding this difference is crucial for pursuing the right treatment strategies. Individuals suffering from GERD should always consult a healthcare provider, particularly if they experience symptoms more than twice a week. These symptoms can profoundly affect daily life, impacting sleep, work, and leisure activities. Some people might find relief through a targeted diet that excludes known irritants. Many individuals report that tomato-based foods and coffee exacerbate symptoms. Keeping a detailed diary documenting meals and symptoms can help individuals pinpoint food triggers more effectively. Furthermore, incorporating regular physical activity into one’s routine is vital. Exercise aids digestion and promotes weight management. However, it is essential to avoid vigorous workouts immediately after meals, as this might worsen symptoms. For those struggling with GERD symptoms, smoking cessation is critical, as tobacco relaxation of the lower esophageal sphincter, which may lead to backflow of acid. In more severe cases, surgical options may be explored.
Medications for Heartburn and GERD
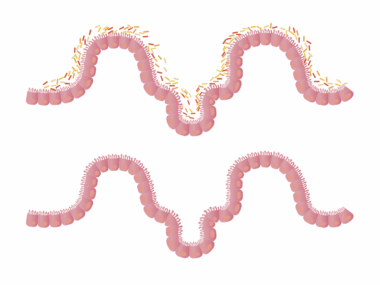
Managing heartburn and GERD often involves a variety of medications designed to reduce acid production in the stomach. Over-the-counter options like antacids, H2 blockers, and proton pump inhibitors (PPIs) can provide relief to many suffering from these conditions. Antacids, typically containing magnesium or calcium, work rapidly to neutralize existing stomach acid. H2 blockers, such as ranitidine or famotidine, are effective in cutting down the production of stomach acid for longer periods. Proton pump inhibitors like omeprazole are often recommended for chronic conditions, as they provide more extended relief. However, long-term use of PPIs should be under medical supervision to avoid potential side effects. It’s vital for patients to discuss their specific situations with healthcare providers. Many may require a tailored approach, starting with lifestyle changes before medication is introduced. In some patients, medications can lead to side effects such as headaches, gastrointestinal upset, or increased risk of certain infections. Awareness of these potential risks is crucial, leading to informed decision-making surrounding treatment. Regular follow-up with a healthcare provider ensures that ongoing management is effective.
In addition to medications, behavioral changes also play a pivotal role in managing heartburn and GERD symptoms. Common recommendations include eating smaller meals more frequently rather than larger ones. This reduces the pressure on the stomach, decreasing the likelihood of acid reflux. Avoiding triggers such as alcohol, caffeine, and acidic foods can minimize symptoms significantly. Maintaining a food diary to log foods consumed and any related symptoms can be beneficial for tracking patterns over time. Hydration is important; consuming adequate water helps with digestion naturally. Some individuals benefit from practicing relaxation techniques, like meditation or yoga, which help mitigate stress, another contributing factor to digestive issues. Stress often leads to poor dietary choices, thus creating a vicious cycle for those suffering from GERD or heartburn. Moreover, limiting food intake before bedtime is recommended. For many, avoiding eating at least three hours before sleeping can lead to substantial symptom relief at night. Patients are encouraged to adopt these lifestyle modifications gradually, allowing their bodies to adjust more effectively.
The Importance of Hydration
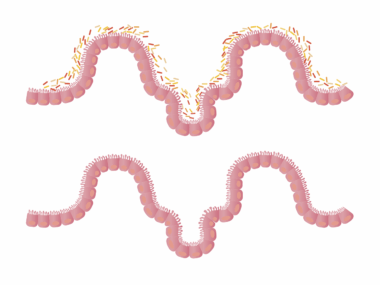
Staying hydrated is essential for gut health, especially for managing conditions like heartburn and GERD. Water plays a crucial role in digestion by helping to dilute stomach acid and facilitate the digestive process. Drinking sufficient water can mitigate some effects of acidity and may help alleviate heartburn symptoms for some individuals. It’s recommended to sip water throughout the day rather than consuming large amounts in one sitting. This approach aids in maintaining optimal stomach acidity levels. Certain beverages, including those containing caffeine or high acidity, can worsen GERD symptoms; therefore, an emphasis on plain water is advisable. Additionally, herbal teas may provide relief and should be considered as alternatives. However, it’s important to choose caffeine-free varieties. Some herbal teas, like chamomile or ginger tea, are particularly soothing for the stomach. Patients should consider their own tolerances when selecting beverages. Another beneficial tip is to use hot water or warm herbal infusions, which can have a relaxing effect on the digestive tract. Ultimately, finding the right balance of hydration is key for effective management of heartburn and GERD.
Besides medication and hydration, proper sleep hygiene also plays a role in managing GERD symptoms. Research indicates that poor sleeping positions can exacerbate heartburn. Elevating the head of the bed by around six to eight inches helps prevent acid from flowing back into the esophagus while sleeping. It’s recommended to avoid sleeping on the right side, as this position may increase the likelihood of experiencing reflux episodes. Maintaining a consistent sleep schedule, where one goes to bed and wakes up at the same time each day, can also improve overall sleep quality. Adequate sleep can reduce stress, which is essential for gut health. High-stress levels have been linked to exacerbated symptoms of GERD and heartburn. Mindfulness techniques such as deep breathing or guided relaxation can also assist in promoting better sleep. Creating a calming bedtime routine that avoids screens and stimulating activities is advisable. Consulting a healthcare professional can provide personalized strategies to manage sleep disturbances. By addressing sleep hygiene, individuals can profoundly improve their overall health and lessen their gastrointestinal symptoms.
When to Seek Professional Help
Determining when to seek professional help for heartburn and GERD is essential for effective management. If you experience chronic symptoms despite lifestyle changes and over-the-counter treatments, it’s crucial to consult a healthcare professional. Signs warranting immediate medical attention include severe chest pain, difficulty swallowing, or unintentional weight loss. These symptoms could indicate more serious underlying conditions, such as esophagitis or Barrett’s esophagus. Additionally, if over-the-counter medications are needed more than twice a week, this might signal a need for prescription-strength treatment or further investigation. Regular follow-ups with healthcare providers help track progress and adjust treatment strategies as necessary. Individuals should feel empowered to discuss their symptoms openly, leading to a more tailored approach to management. Educating oneself about symptoms, triggers, and potential treatment options can facilitate better conversations with healthcare professionals. Before any changes are made to the treatment plan, seeking guidance is strongly advised. In many cases, early intervention can prevent the condition from worsening, ensuring a better quality of life.
In conclusion, heartburn and GERD are manageable conditions that require a multifaceted approach. Lifestyle changes, including dietary modifications, stress management, and proper sleep hygiene, all contribute to improved gut health. Medications can offer significant relief but should be used judiciously and under guidance. Staying hydrated, understanding personal triggers, and seeking professional help when necessary are essential strategies for effective management. By integrating these practices into daily routines, individuals experiencing heartburn and GERD can enjoy a better quality of life. Furthermore, commitment to regular health check-ups can assist in monitoring progress and adjusting treatment plans. Incorporating supportive communities and resources, such as online forums or local support groups, can provide added motivation and advice during challenging times. Engage with others experiencing similar health challenges can foster a sense of belonging and understanding. Ultimately, effective management of heartburn and GERD is a collaborative effort, combining personal responsibility with professional guidance. Embracing a proactive attitude towards gut health will lead to long-term benefits and overall well-being. Employing these strategies consistently can pave the way for relief and a healthier, more active lifestyle.