How to Access Emergency Medical Help When You Have Diabetes
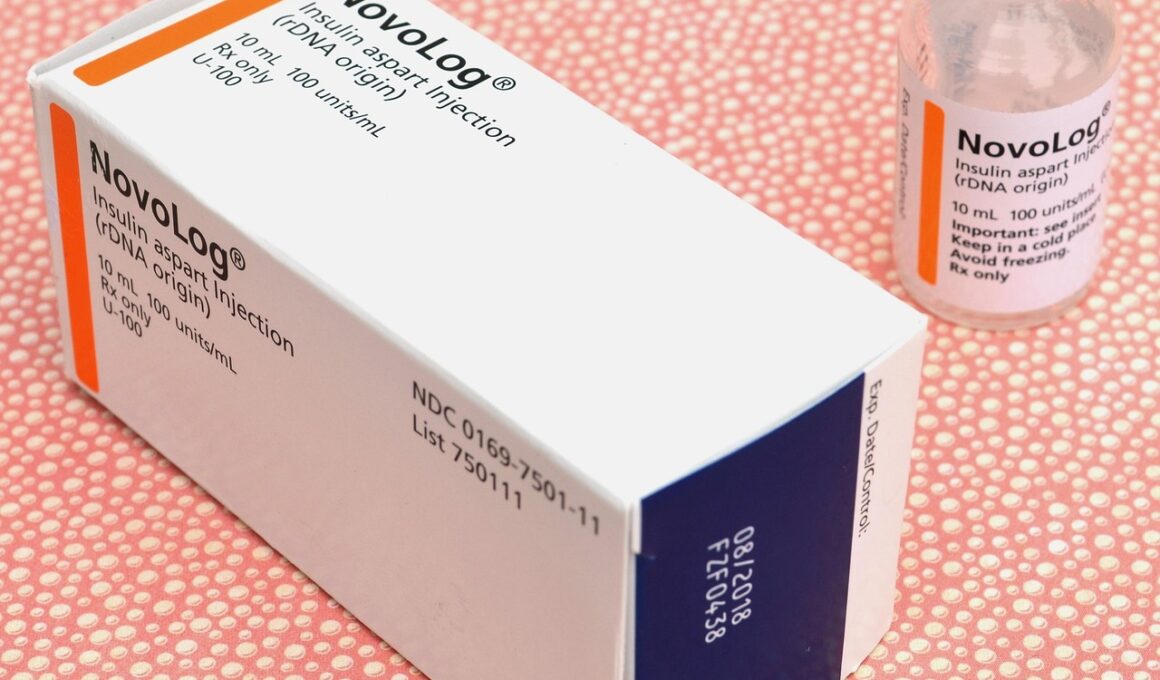
If you are diabetic, it is crucial to prepare for emergencies where medical assistance might be needed urgently. One of the most important factors is to always wear a medical ID. This alert can provide vital information about your condition to first responders if you’re unable to communicate. Choose ID items like bracelets or necklaces that are clearly marked and designed to withstand everyday activities. Stock your emergency bag with essential supplies such as snacks that raise blood sugar, a glucose meter, and a backup supply of insulin. Educate family and friends about your diabetes management plan. Make sure they understand how to recognize symptoms of hypoglycemia or hyperglycemia. Keeping them informed will facilitate quicker action should an emergency occur. Consider downloading health apps that communicate your health information with emergency services. It can save precious time during a crisis. Familiarize yourself with the nearest emergency medical facilities that are equipped to deal with diabetes-related issues. Awareness of their protocols can enable you to seek appropriate help swiftly in a dire situation. Remember that being prepared significantly enhances your chances of effective, timely treatment when you’re in distress.
Communication with healthcare providers is crucial, particularly in emergency situations. Keep an updated list of your medications, allergies, and emergency contacts. Share this information with trusted individuals who can relay details when needed. Having a clear electronic record can be beneficial in emergencies. Use a secure health app that maintains all your health records easily accessible to authorized medical personnel when required. This accessibility can speed up assessments and care during critical moments. Training in basic emergency response for yourself and your close contacts enhances your safety. Take part in workshops or courses on first aid and CPR, focusing more on diabetic emergencies. Understanding blood sugar fluctuations, recognizing symptoms, and knowing potential complications equips you to respond effectively. Prioritize discussions with your doctor regarding your emergency action plan. Create an outline that clearly explains necessary steps if a severe incident occurs, such as when to use glucagon or when to seek medical treatment. Sticking to a well-defined protocol saves panic and confusion during emergencies. Ensure everyone involved is aware of your action plan, maintaining a sense of readiness.
Identifying Symptoms of Emergencies
Recognizing early symptoms of diabetes-related emergencies can be vital in averting severe complications. Hypoglycemia, or low blood sugar, often presents with symptoms like dizziness, confusion, shaking, and sweating. Conversely, hyperglycemia, or high blood sugar, can cause excessive thirst, frequent urination, fatigue, and blurred vision. Being astute to these symptoms and acting swiftly is essential in emergency situations. Carry fast-acting carbohydrates such as glucose tablets or juice boxes at all times. These items can counteract low blood sugar levels quickly and effectively. If you notice early hypoglycemic signs, consume these carbohydrates immediately to mitigate the symptoms. Remember that untreated hypoglycemia can lead to confusion, seizure, or loss of consciousness. On the other hand, if struggling with hyperglycemia, ensure you have a reliable method to administer insulin if prescribed. Be cautious with escalating symptoms, as they may lead to diabetic ketoacidosis or hyperglycemic hyperosmolar syndrome. Seek medical attention as necessary. Tracking changes in your body helps maintain awareness. Regularly monitoring your blood sugar levels can assist in noticing sudden fluctuations and help keep you safe in emergencies.
Staying informed about local emergency resources is a vital aspect of being prepared. Research nearby hospitals, urgent care centers, or clinics that specialize in diabetes care. Compile a list of resources including their contact details and addresses, storing them in an easy-to-access location. Make sure your phone has all emergency contact numbers saved, including family, friends, and local doctors. During an emergency, you can quickly call upon these people for assistance. Moreover, sign up for local alerts or communication channels that share valuable information regarding medical resources during crises. Many organizations provide text alerts or app notifications about available services for diabetics during emergencies. Consider downloading any apps that allow direct communication with healthcare providers. There are various telehealth options that enable consultations even when you cannot reach facilities. Ensure you also have resources about food and exercise management in crisis periods. Knowing how specific foods affect your blood sugar can guide decisions during emergencies, ensuring you maintain optimal health in rapid-response environments. Remember, knowledgeable preparation can make a substantial difference in critical situations.
Creating a Personal Emergency Plan
Establishing a personalized emergency plan is a significant step towards preparedness. Engage with your healthcare provider to build a comprehensive strategy tailored to your unique situation. Outline necessary routines for blood sugar monitoring, food consumption, and medication administration. Your plan should also include instructions for loved ones on how to assist you during an emergency. Write down situations that require immediate assistance and appropriate responses. For instance, clarify when to administer glucagon or when to seek outside help. Share this plan with close family members, caregivers, and friends to ensure they are aware of it. Moreover, evaluate your plan periodically, updating it as necessary to reflect any lifestyle changes or new medical advice you receive. Rehearsing your response plan with your support network can build confidence and understanding among everyone involved. Consider preparing a document that includes emergency contacts, medical history, and treatment preferences, keeping it easily accessible. In addition to physical documents, look into utilizing digital solutions for documenting essential information, aiding quicker access when required during emergencies as well. Always be prepared to adapt your plan as situations change.
Traveling poses unique challenges for those with diabetes, necessitating additional preparations. Before heading out, ensure all necessary medications and supplies are securely packed and easily accessible. Carry sufficient supplies to cover the duration of your trip, plus extras in case of unforeseen delays. Labeling items can prevent mix-ups with others’ medications. Stay informed about your destinations, particularly concerning healthcare facilities. Know the locations of clinics and hospitals nearby, along with their operating hours. Use technology to assist: mobile apps can help locate nearby pharmacies or urgent care centers. Moreover, communicate your condition and needs in advance if you’re traveling with a group. Let fellow travelers know how to respond should an emergency arise. Always have at least one identifiable person accompany you during outings who understands your diabetes management. Create a checklist of essentials for each trip that includes snacks, blood sugar logs, syringes, and emergency contacts. Aside from medical needs, always remember to consider the presence of stress or dietary changes, as they can lead to fluctuations in blood sugar. Maintaining vigilance will help keep your diabetes management steady during travel.
Conclusion: Empower Yourself with Knowledge
Empowering yourself with knowledge is paramount for effectively accessing emergency medical help while managing diabetes. The strategies discussed play a fundamental role in ensuring your safety and well-being. Regularly reviewing medical plans, preparing emergency kits, maintaining adequate communication, and identifying local resources are critical steps. Knowledge of your body’s signals can lead to swift and effective action during unforeseen circumstances. Understanding emergency protocols can contribute to minimizing crisis impact and anxiety. Share information about diabetes management with loved ones and encourage them to participate in training sessions, enhancing their ability to provide help. Remember, preparation, education, and collaboration with healthcare providers lead to better outcomes. Ensuring continuous communication with your healthcare team can help adjust treatment plans, addressing changing needs proactively. Know your specific medical rights and access points, reinforcing your ability to seek help without hesitation. Lastly, regularly review new developments in diabetes management options, ensuring informed decision-making is possible even in emergencies. By actively taking these steps, you not only enhance your well-being but also inspire others in your community to prioritize their preparedness when facing similar challenges.
Your health is your responsibility, and taking proactive steps to prepare for emergencies can increase your confidence in managing your diabetes effectively. Being well-prepared helps you tackle challenges and reinforces your commitment to health. Stay informed and connected with your healthcare network, contributing to your overall wellness. Equip yourself with practical skills and knowledge, enabling you to face any situation that arises with resilience and foresight. Actively engaging in personal preparation leads to a sense of empowerment, ensuring that you don’t face emergencies unprepared. When you understand the resources available and take concerted steps towards readiness, your ability to maintain health remains a priority under duress. Consider this an opportunity to focus on your health and transform challenges into lessons and growth. Reinforce your self-efficacy through regular evaluations of your emergency plan, keeping yourself and your support team sharp and informed. As you weave emergency preparedness into your daily life, recognize the impact on your overall quality of life. Embrace the role of a proactive participant in your health and well-being. Always remember, that peace of mind starts with preparation and knowledge.