Pros and Cons of Fasting for Gut Microbiome Balance
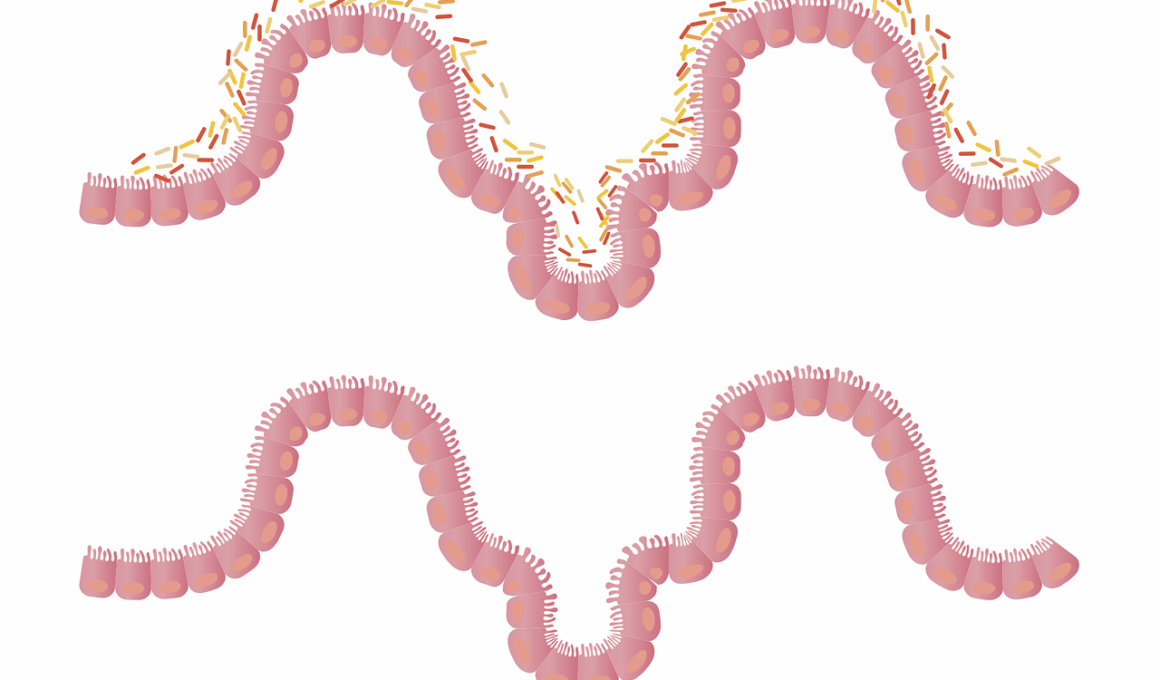
Fasting has gained popularity for its potential health benefits, especially regarding gut microbiome balance. This balance is crucial as the microbiome plays a significant role in digestion, immune function, and overall gut health. Regular intermittent fasting can help diversify gut bacteria, promoting a more resilient microbiome. Researchers suggest that when fasting, the body goes through a cleansing process. This process can potentially help eliminate harmful bacteria and facilitate the growth of beneficial strains. For instance, shorter fasting windows might support the proliferation of lactobacilli, crucial for maintaining gut equilibrium. However, it is also essential to consider the possible downsides. Extreme fasting can disrupt the microbiome, leading to decreased diversity. This reduction could compromise gut health, resulting in digestive issues or increased inflammation. Additionally, fasting can negatively influence individuals with pre-existing health conditions. As such, the impact of fasting on gut microbiome balance can vary tremendously between individuals. Some may benefit significantly, while others may experience adverse effects. Therefore, it’s essential to approach fasting mindfully, ensuring a balanced diet integrated into the fasting approach to maximize benefits for gut health.
Understanding Fasting and Its Effects
Fasting typically involves abstaining from food for a specific period, which can vary widely. There are several methods to consider, including intermittent fasting, where individuals cycle between periods of eating and fasting. This approach allows the body to enter a state of autophagy, promoting cellular repair and potentially benefiting gut health. During this time, gut bacteria can reset, leading to a shift in composition. Many studies indicate that fasting assists in regulating blood sugar levels, which can further positively influence the gut microbiome. Fasting can lead to the production of short-chain fatty acids (SCFAs) through fermentation by gut bacteria when nutrients are scarce. SCFAs are essential for gut health, reducing inflammation and supporting the intestinal barrier. Furthermore, fasting might help alleviate symptoms associated with gastrointestinal disorders like irritable bowel syndrome (IBS) by allowing the gut to rest and heal. Not everyone, however, will experience these benefits. Individuals consuming highly processed foods before fasting may not see significant improvements as their gut microbiome could be heavily imbalanced. Personalized dietary adjustments are therefore recommended alongside fasting to ensure optimal benefits while considering individual health conditions and dietary preferences.
While exploring the connection between fasting and the gut microbiome, it is crucial to consider the timing of food intake. This means focusing not only on when to eat but also on what to eat when one breaks the fast. Consuming a diet rich in fiber, healthy fats, and probiotics can greatly enhance fasting benefits on gut microbiome balance. Foods like fruits, vegetables, whole grains, and fermented products can support beneficial bacteria growth. Conversely, diets high in sugars and unhealthy fats can have detrimental effects. If the post-fasting diet lacks essential nutrients, it may nullify the positive effects of fasting, potentially causing more harm than good to gut health. Additionally, hydration also plays a vital role during both fasting and non-fasting periods. Prolonged dehydration can alter gut microbiota adversely, leading to discomfort and digestive issues. Therefore, it’s essential to plan meals carefully after fasting to ensure they contribute positively to the microbiome. Meal timing and composition can essentially act as powerful tools for anyone looking to utilize fasting to improve gut health effectively.
Scientific research into fasting and the gut microbiome has expanded in recent years, revealing various mechanisms through which fasting could enhance gut health. One notable aspect is the impact of fasting on the immune system, which is closely linked to the gut microbiome. The gut-associated lymphoid tissue (GALT) plays a critical role in maintaining immune responses, and fasting may help strengthen this connection. During fasting, the body can shift its energy sources, enabling it to utilize fat stores. This adaptation could potentially lead to an improvement in gut microbiome resilience by providing an environment conducive to beneficial bacteria. Furthermore, fasting can also affect gut motility and ease inflammation throughout the digestive tract, leading to improvements in conditions like Crohn’s disease or ulcerative colitis. Given that the balance of gut bacteria is essential for maintaining good health, the combined effects of fasting on inflammation and immune function can significantly improve overall gut health. Still, while many advocate for fasting, it’s essential to remember that results vary, and personal experiences may differ. Therefore, consultation with a healthcare professional before embarking on any fasting regimen is critical.
Another significant factor to consider in the discussion of fasting and gut health is the influence of age and lifestyle. Older adults may experience different effects from fasting compared to younger individuals due to changes in metabolism and gut microbiome composition over time. As people age, the diversity of gut microbiota often decreases, which may impact how fasting influences gut balance. Similarly, lifestyle factors and dietary habits play an important role. People with higher stress levels or those not consuming balanced diets may not experience the same results as those who lead healthier lifestyles. Stress negatively affects gut health, potentially destabilizing the microbiome regardless of fasting practices. Therefore, addressing lifestyle elements like stress management, sleep, and physical activity becomes crucial. Adopting a holistic approach that integrates these factors will likely yield better long-term effects on gut microbiome health. In this respect, fasting can be viewed not as a standalone solution but as a part of an overall wellness strategy. Individuals should view fasting as a tool that can work harmoniously with other healthy lifestyle choices to enhance gut well-being.
Conclusion: The Path Forward for Fasting and Gut Health
In conclusion, the relationship between fasting and gut microbiome health is complex and multifaceted. Research suggests that there are both benefits and risks associated with fasting as it pertains to gut microbiome balance. While many individuals may find positive improvements, others could experience negative consequences if fasting is done improperly or without proper dietary support. This underscores the necessity of tailored approaches to fasting and gut health management. Practitioners must consider individual health backgrounds while providing advice. Emphasizing a balanced approach that combines mindful fasting with a nutrient-dense diet can provide a path to improved gut health. Furthermore, ongoing research is essential to better understand the mechanisms at play and how to optimize fasting practices. As more studies emerge, they will guide individuals seeking to improve their gut microbiome. Additionally, educating individuals on the importance of maintaining diversification within their gut microbiome is vital. Recognizing the subtle interplay between diet, fasting, and gut health can ultimately empower people to make informed decisions about their health. By taking an integrated approach, one can genuinely harness the potential of fasting to benefit gut microbiome balance.
Ultimately, the potential of fasting for promoting gut microbiome balance offers exciting opportunities for health improvement. Adopting this practice can initiate significant changes within the gut, leading to better overall health outcomes. As more research sheds light on specific strategies, such as the timing and types of food intake, individuals can harness fasting to enhance their gut health meaningfully. The advent of personalized nutrition protocols may transform how we perceive fasting and dietary approaches in general. Therefore, individuals should not only explore fasting practices but also remain open to adapting them according to their evolving health needs. Continuing to engage with healthcare professionals and nutritionists can provide support and guidance during this journey. Thus, integrating knowledge about gut microbiome balance with daily dietary choices empowers individuals to take charge of their health. As society becomes increasingly aware of the importance of gut health, fasting could become one of the many effective strategies to achieve optimal wellness. By focusing on a healthy lifestyle, nutrition, and fasting, individuals can navigate their paths toward better gut health and overall well-being.
Ultimately, recognizing the synergistic relationship between fasting and gut microbiome balance can enhance overall health. Progress requires understanding, experimentation, and balance in the approach to fasting. Personalizing fasting methods while remaining aware of individual needs will facilitate optimal gut health improvements. Therefore, it’s essential for future studies to focus on validating findings and refining methods. The more we learn about the gut microbiome’s complexities, the better equipped we will become to make informed health decisions. Knowledge is power, and it is vital to continue exploring and understanding the advantages and potential risks of fasting. Individuals should feel empowered to take a proactive stance toward their health, making dietary choices that support their gut microbiome while integrating fasting practices thoughtfully in their lives. In this respect, fasting can be a powerful tool when applied in harmony with overall health strategies, providing individuals the opportunity to enhance their gut microbiome balance while promoting well-being.