The Impact of Antibiotics on Your Child’s Gut Microbiome
In today’s world, children often receive antibiotics, crucial for treating bacterial infections. However, the impact of these antibiotics extends beyond just fighting disease. Research suggests that antibiotics can significantly alter a child’s gut microbiome, which comprises trillions of microorganisms crucial for health. This disruption can lead to short-term effects like digestive issues or long-term consequences such as autoimmune diseases and obesity. It’s essential to understand the implications of antibiotics on the gut as early childhood is a vital period for microbiome development. The gut microbiome influences various bodily functions, including digestion and immune responses. When antibiotics are administered, they can wipe out beneficial bacteria alongside harmful ones. This can create an imbalance that impairs gut health, potentially leading to increased susceptibility to infections and a range of health problems later on. Parents should be cautious about overusing antibiotics, recognizing their role in promoting a healthier gut microbiome. Consulting healthcare professionals about necessary medications and exploring alternatives where appropriate can help maintain your child’s gut health while effectively treating infections.
Understanding the Gut Microbiome
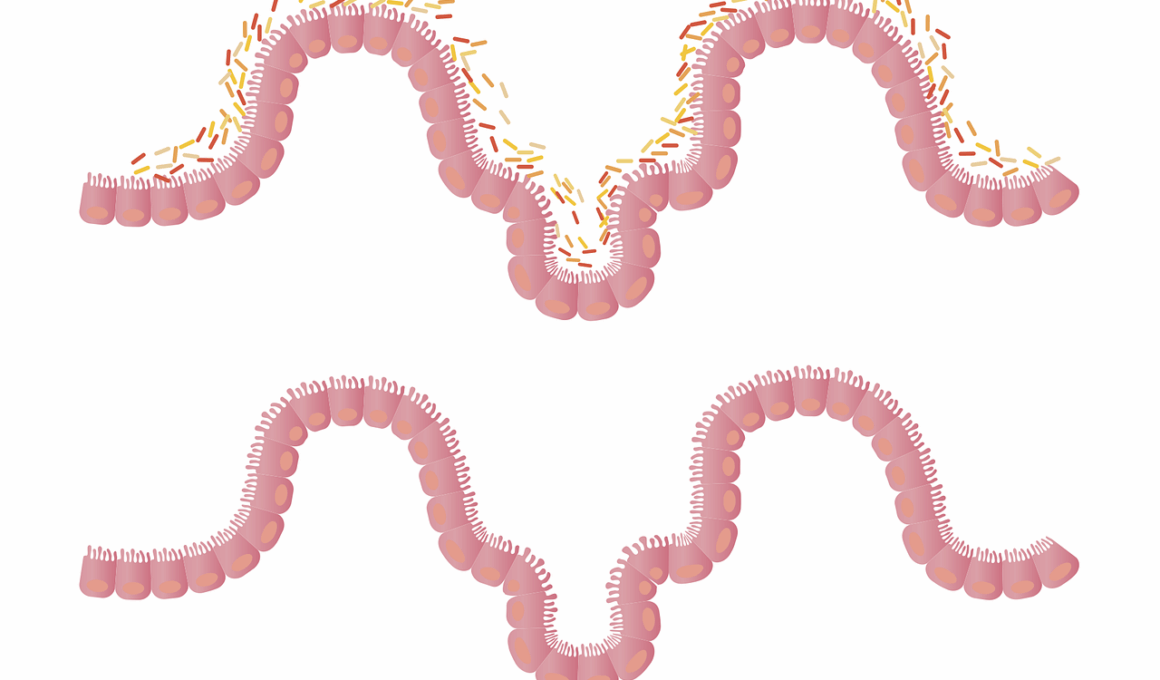
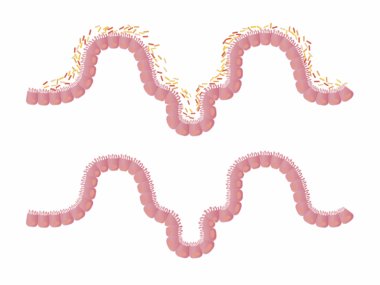
The gut microbiome is a complex ecosystem that plays a vital role in nutrition and health. It consists of diverse bacteria, fungi, viruses, and other microbes that coexist symbiotically within the gastrointestinal tract. This ecosystem is crucial for various functions such as digestion, metabolism, and immune regulation. Healthy microbiomes are diverse, with numerous species contributing to a balanced system; however, antibiotic use can drastically change this environment. The shift typically results in a decrease in microbial diversity. A less diverse microbiome may lead to dysbiosis, a condition associated with digestive disorders, allergies, and obesity. Studies indicate that children receiving antibiotics early in life are at a higher risk of developing such issues. This highlights the importance of protecting children’s microbiomes during their formative years. Parents can support this system through a healthy diet rich in fiber and probiotics. Introducing fermented foods can help replenish beneficial bacteria after antibiotic use. Overall, understanding the gut microbiome encourages respect for its delicate balance, linking the use of antibiotics to broader health implications, emphasizing the necessity of mindful practices in treating young individuals.
When antibiotics are necessary, timing and dosage become critical factors. Research indicates that the timing of antibiotic administration can affect the development of a child’s gut microbiome. For instance, early-life exposure to antibiotics can lead to significant shifts in microbial composition, while exposure later on may have different effects. Careful consideration of the type and length of antibiotic course is crucial. Short courses of narrow-spectrum antibiotics are generally less disruptive than broad-spectrum ones. Parents and healthcare providers should weigh the benefits of antibiotics against the potential long-term effects on gut health. Understanding the need for individualized treatment plans based on specific health conditions can aid in reducing unnecessary antibiotic prescriptions. Moreover, recent studies suggest that restoring gut health post-antibiotic treatment is as essential as the treatment itself. Incorporating prebiotics and probiotics into a child’s diet can help reestablish a healthy microbiome. It is important to discuss these options with healthcare professionals while monitoring the child’s health closely. Maintaining communication between parents and healthcare providers can lead to better-informed decisions regarding the use of antibiotics in children.
Long-Term Effects of Antibiotic Use
The long-term effects of antibiotic use in childhood can manifest in numerous ways, shaping a child’s health trajectory. Studies link early antibiotic exposure to increased risks of allergies, asthma, and metabolic disorders as they grow. For example, children with disrupted microbiomes may experience altered immune responses, resulting in higher susceptibility to infections and autoimmune diseases. Additionally, there are concerns about the relationship between antibiotic use and obesity development in children. Antibiotic-induced microbiome changes can affect metabolism and appetite regulation. This association has sparked interest in exploring preventive measures against such outcomes. Research into alternatives to antibiotics, such as bacteriophages and targeted therapies, is ongoing and shows promise. Ensuring appropriate usage of antibiotics while considering these long-term impacts should be a priority for parents and healthcare professionals. Furthermore, public health campaigns emphasizing responsible antibiotic use can significantly reduce the likelihood of developing antibiotic resistance. Awareness, education, and preventive strategies are essential in mitigating the adverse effects on children’s health stemming from unnecessary antibiotic treatment, fostering healthier futures among the next generation.
In addition to dietary interventions, another approach is to advocate for prescriber responsibility. This involves educating healthcare providers about the ramifications of antibiotic prescribing patterns as they pertain to gut health. An increased awareness of childhood microbiome development can prompt providers to consider non-antibiotic treatments whenever possible and emphasize recovery strategies afterward. Research findings should be disseminated widely through seminars and continuing medical education, ultimately translating into better practices in pediatric care. Moreover, parents can play a pivotal role by remaining knowledgeable about their children’s antibiotic prescriptions and questioning when necessary. A collaborative effort between families and health practitioners will bolster positive outcomes in preserving gut diversity. Fostering a proactive stance towards gut health can empower parents, guiding them in making informed decisions that enhance their child’s overall well-being. Maintaining values of health literacy within communities and promoting access to resources that support gut health can lead to more robust microbiomes across populations. The collective engagement of parents, professionals, and researchers can create effective strategies to protect children’s gut microbiomes.
Restoring Gut Health After Antibiotic Treatment
Restoration of gut health post-antibiotic treatment is crucial for maintaining a balanced microbiome in children. One effective method is the introduction of probiotics, which are beneficial live bacteria that can help recolonize the gut. Fermented foods like yogurt, kefir, and sauerkraut are excellent sources of probiotics. Parents should consider incorporating these foods into their child’s diet after a course of antibiotics. In addition to probiotics, prebiotics can also play a significant role. Prebiotics are dietary fibers that feed beneficial gut bacteria, enhancing their growth and activity. Foods rich in prebiotics, such as bananas, onions, garlic, and whole grains, should be included regularly. These combined strategies help restore the gut’s microbial balance and reduce the risks associated with dysbiosis. Consultation with a healthcare provider can guide parents in selecting appropriate probiotic supplements tailored for children, ensuring a safe and effective process. Staying hydrated is equally important, as water facilitates overall digestive health. Maintaining a balanced diet contributes greatly to the child’s recovery post-antibiotic treatment and offers support to restore optimal gut function effectively.
Finally, creating a healthy environment for children can greatly impact their gut microbiome. This involves fostering physical activity, ensuring good sleep, and reducing stressors, all of which are essential components of overall health. Regular physical activity has been linked to increased microbiome diversity, which is beneficial in combatting age-related and antibiotic-induced dysbiosis. Additionally, adequate sleep allows the body’s systems to recover and function optimally, further supporting gut health. Parents can cultivate supportive processes by encouraging outdoor play, limiting screen time, and nurturing strong social connections through structured activities. When children experience lower stress levels, their gut microbiomes benefit, resulting in better digestion and immune responses. Furthermore, ongoing education is vital; parents must remain informed about current research in this area. By engaging with healthcare providers, families can explore new insights and stay updated on best practices for fostering gut health. The synergy between a nurturing environment, informed dietary choices, and healthcare collaboration will ultimately enhance microbiome resilience, paving the way for healthier childhood development and a brighter future.
In conclusion, the impact of antibiotics on a child’s gut microbiome is profound and multifaceted. As children are among the most frequent recipients of antibiotics, understanding these implications is crucial. Parents and healthcare providers must work together to ensure that antibiotics are prescribed only when necessary and coupled with strategies to protect and restore gut health. Emphasizing diet and lifestyle changes can significantly enhance recovery and promote a flourishing microbiome. Supporting the gut’s ecosystem through various interventions—such as probiotics and prebiotics—will help ensure long-term health benefits. Furthermore, nurturing a healthy environment contributes significantly to the overall gut health of a child, forming a protective layer against potential adverse effects of antibiotic use. By cultivating awareness around gut microbiome development and the importance of maintaining its health, communities can develop stronger, healthier generations. Ultimately, it’s about a collective commitment to shaping a healthier future for children, guided by knowledge and proactive choices regarding antibiotics, microbiomes, and their intertwined destinies in our ever-evolving world.