The Role of Gut Microbiome in IBS-Related Fatigue and Brain Fog
The gut microbiome plays a crucial role in overall health, influencing digestive processes, immune function, and even mental health. Individuals suffering from Irritable Bowel Syndrome (IBS) often experience symptoms beyond gastrointestinal discomfort, including debilitating fatigue and brain fog. Recent studies suggest that the gut microbiome’s composition and functionality significantly impact these extra-intestinal manifestations. Dysbiosis, or an imbalance in the gut microbiota, can lead to inflammation and altered neurotransmitter levels, exacerbating fatigue and cognitive dysfunction. A thriving, balanced microbiome supports efficient nutrient absorption and minimizes inflammation, directly influencing energy levels. Maintaining a healthy gut may help alleviate these frustrating symptoms, leading to improved overall quality of life. Additionally, a diverse microbiome can enhance resilience against stress, essential for managing the psychological stresses of living with IBS. As scientists continue to explore the intricate link between the gut and brain, targeted interventions, including dietary adjustments and probiotics, may offer promising pathways to tackle IBS-related fatigue and brain fog more effectively. An integrated approach encompassing gut health could lead to innovative strategies towards managing these challenging IBS symptoms.
Understanding IBS and Its Symptoms
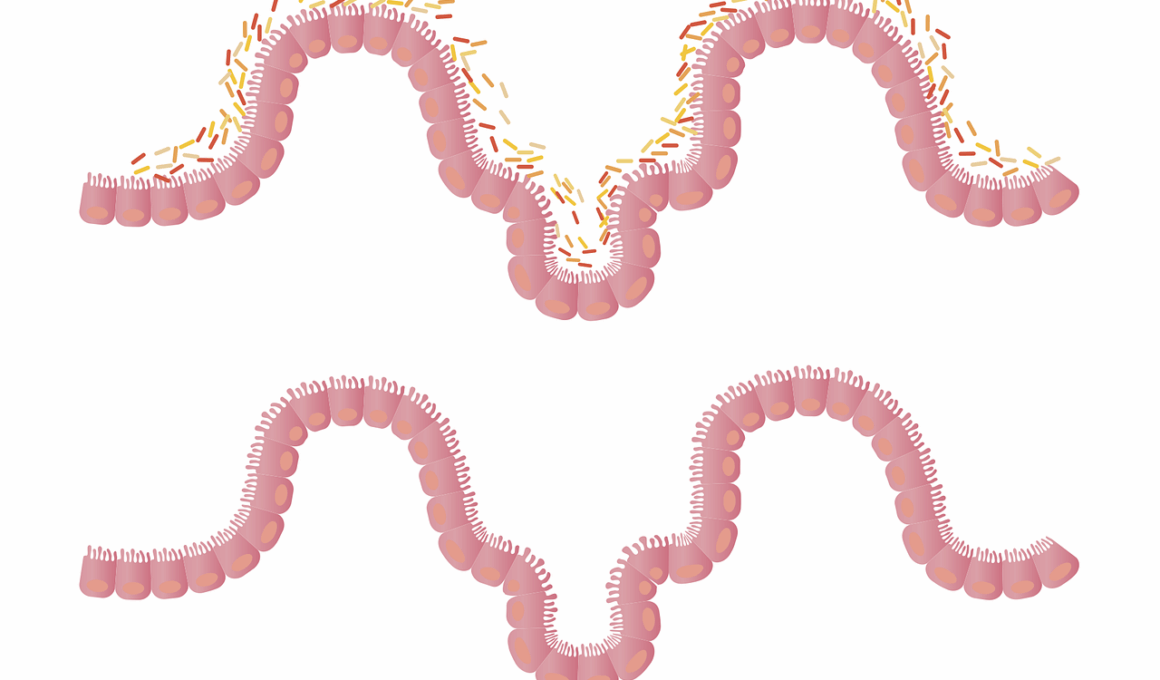
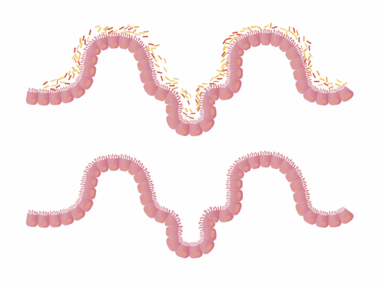
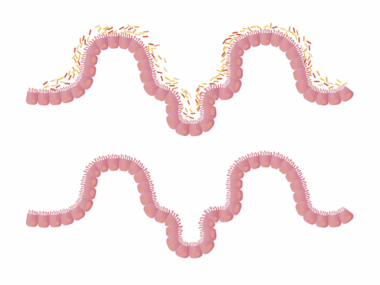
Irritable Bowel Syndrome, commonly known as IBS, encompasses a range of gastrointestinal symptoms affecting a significant portion of the global population. Characterized by abdominal pain, bloating, diarrhea, and constipation, IBS often takes a toll on individuals’ daily lives. However, symptoms frequently extend beyond the gut, manifesting as fatigue and brain fog. These symptoms can severely impact the ability to perform at work or engage in social activities, leading to frustration and emotional distress. While the precise cause of IBS remains elusive, it is thought to involve factors such as gut motility, sensitivity, and inflammation. Importantly, the gut microbiome’s role in IBS is gaining attention, as it interacts with both the intestinal lining and the nervous system. Studies highlight the potential impact of gut bacteria on the brain, illustrating how dysbiosis may exacerbate mental fatigue and cognitive impairments. Incorporating dietary changes and improving gut health may offer promising strategies to manage IBS more effectively, potentially reducing the incidence of fatigue and brain fog. Further research is essential to understand the complete relationship between gut health, IBS, and related symptoms.
Microbiome Diversity and Its Significance
A diverse microbiome is essential for maintaining gut health and improving overall well-being. In individuals with IBS, the balance among various gut bacteria can become disrupted. This dysbiosis can lead to inflammation, which plays a pivotal role in the gut-brain axis, influencing cognitive functions and emotional health. Microbiome diversity contributes to optimal digestion and absorption of nutrients, essential for energy metabolism. When the gut microbiota is diverse, it can effectively modulate the immune system and produce short-chain fatty acids, which are vital for gut health and have anti-inflammatory properties. Low microbial diversity has been linked to IBS symptoms, including fatigue and cognitive issues. To promote microbiome diversity, individuals can consider dietary modifications, such as including prebiotics and probiotics, reducing processed food intake, and emphasizing whole foods rich in fiber. Additionally, lifestyle factors such as daily physical activity can further enhance microbiome health. Increased awareness and understanding of the gut microbiome’s importance urge individuals with IBS to examine their dietary habits thoughtfully. This, in turn, can empower them to combat fatigue and brain fog symptoms linked to their condition.
Dietary Interventions for IBS Management
Implementing specific dietary interventions may greatly influence the management of IBS symptoms. Research suggests that dietary approaches, such as the FODMAP diet, can effectively reduce IBS-related discomfort. The low-FODMAP diet involves minimizing fermentable carbohydrates that can trigger symptoms such as bloating, gas, and abdominal pain. By conducting an elimination phase and gradually reintroducing specific foods, individuals can identify triggers and personalize their diet accordingly. Additionally, increasing fiber intake from fruits, vegetables, and whole grains can support a healthy microbiome and alleviate constipation, a common IBS symptom. Fermented foods, such as yogurt, kefir, and sauerkraut, can also introduce beneficial bacteria to the gut and enhance diversity. Regular hydration is equally crucial, as it supports digestive processes and overall health. Individuals suffering from IBS-related fatigue should consider food choices that enhance energy without causing gastrointestinal upset. It is essential to work with healthcare providers or registered dietitians to develop tailored dietary plans that suit individual needs. Comprehensive dietary management can lead to significant improvements in IBS symptoms and overall well-being, allowing individuals to regain control of their health.
Probiotics and Their Role in IBS Treatment
Probiotics are live microorganisms that can confer health benefits when consumed in adequate amounts. Their role in managing IBS symptoms, specifically fatigue and brain fog, is a growing area of research. Probiotics can help restore the balance of the gut microbiome, which is often disrupted in individuals with IBS. Certain strains, such as Lactobacillus and Bifidobacterium, have shown promise in alleviating IBS symptoms. Studies indicate that probiotics may reduce bloating, improve stool consistency, and enhance the overall quality of life for IBS patients. In addition, probiotics can exert positive effects on the gut-brain axis, potentially improving cognitive function and mood. Incorporating fermented foods rich in probiotics, like kimchi and yogurt, into the diet may support gut health. Additionally, choosing probiotic supplements with proven efficacy and appropriate strains is crucial for optimal results. Consulting with healthcare professionals can help individuals identify suitable probiotic options tailored to specific needs. Overall, the integration of probiotics into treatment plans may serve as an effective strategy to reduce IBS-related fatigue and brain fog.
The Gut-Brain Axis Connection
The gut-brain axis is a complex communication network linking the gut and the brain, influencing various bodily functions, including mood, behavior, and cognitive processes. This connection is vital in understanding IBS, particularly concerning fatigue and brain fog. Research indicates that the gut microbiome can communicate with the central nervous system, impacting neurotransmitter levels such as serotonin, which plays a crucial role in mood regulation. Dysbiosis can lead to increased intestinal permeability and inflammation, further exacerbating cognitive symptoms associated with IBS. Stress can also influence this connection significantly, as emotional distress can alter gut motility and microbiome composition. Consequently, managing stress through relaxation techniques, mindfulness, and yoga may aid in restoring the gut-brain balance. Furthermore, dietary habits and microbiome health can be enhanced to support this system effectively. Lifestyle modifications that promote a healthy gut microbiome can improve both gastrointestinal and neurological symptoms. Understanding the gut-brain axis’s role in IBS empowers individuals suffering from fatigue and brain fog to adopt holistic strategies for symptom management, fostering improved quality of life.
New Research Directions and Future Perspectives
The relationship between the gut microbiome and IBS presents exciting research opportunities. Emerging studies focus on understanding how gut bacteria influence brain function, potentially leading to innovative treatments for fatigue and cognitive symptoms. Ongoing clinical trials are investigating targeted probiotic therapies tailored to individual microbiome profiles, exploring personalized medicine for IBS management. Furthermore, researchers are examining the role of diet, prebiotics, and the influence of dietary patterns on the gut microbiome over time. Understanding individual bacterial profiles may unveil unique insights into effective treatment options, enhancing the management of IBS symptoms, fatigue, and brain fog. Moreover, the potential of fecal microbiota transplantation (FMT) is being studied as a treatment for IBS, which may revolutionize future approaches. As our knowledge of the gut microbiome expands, comprehensive strategies encompassing lifestyle, dietary changes, and microbiome testing will become more prevalent. Patients and healthcare providers must remain informed about these developments to implement novel approaches proactively. Research in this field holds great promise for offering new hope in addressing the multifaceted challenges faced by individuals with IBS, allowing for better management of fatigue and cognitive dysfunction.
Conclusion: The Path to Better Health
In conclusion, the role of the gut microbiome in IBS-related fatigue and brain fog highlights the intricate link between digestive health and mental well-being. Individuals suffering from IBS should consider comprehensive management strategies, addressing both gastrointestinal and cognitive symptoms holistically. By focusing on dietary interventions, probiotics, and lifestyle modifications, it may be possible to restore balance to the gut microbiome, mitigate inflammation, and enhance energy levels. Furthermore, understanding the gut-brain axis’s role can empower patients to make informed decisions regarding their health and well-being. With ongoing research and advancements in the field, new approaches may arise, improving the quality of life for those navigating the complex landscape of IBS. It is essential for individuals to work closely with healthcare professionals to develop personalized treatment plans that cater to their unique circumstances. A proactive approach that encompasses both physical and mental health aspects can pave the way towards resilience and vitality. Ultimately, the journey to a healthier gut microbiome can reduce fatigue and cognitive dysfunction, fostering better health outcomes for individuals with IBS.