The Impact of Diabetes Medications on Weight and Appetite
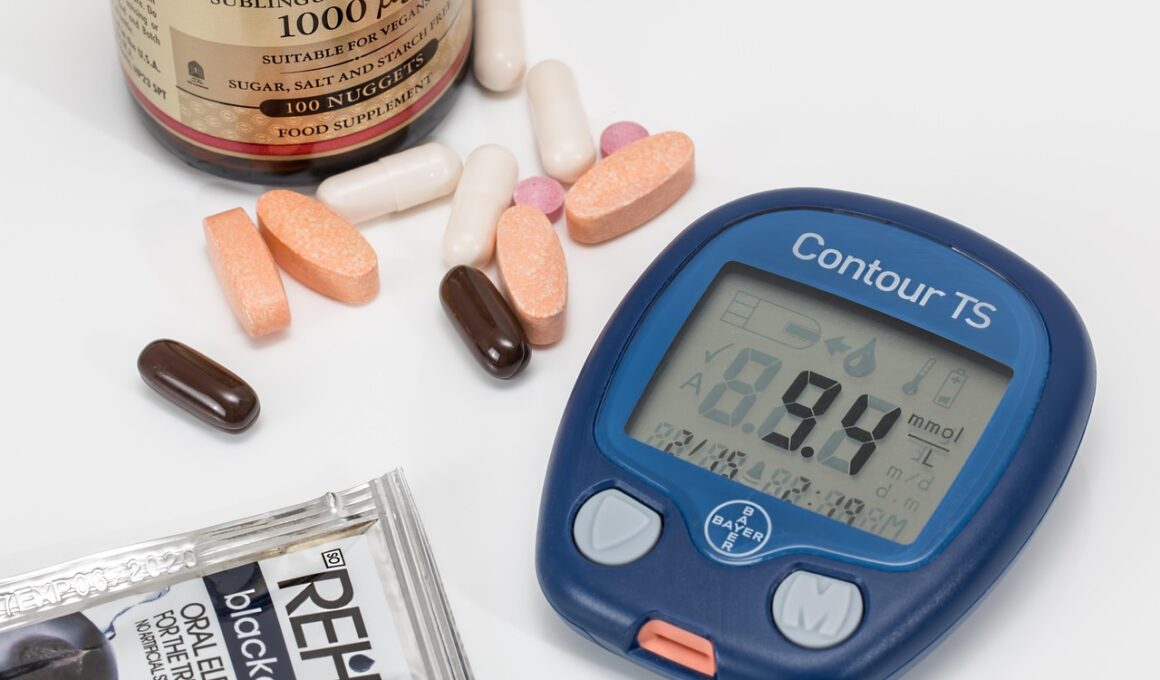
Diabetes medications can significantly influence both weight and appetite in individuals managing this chronic condition. Understanding these effects is vital for comprehensive diabetes care. Various classes of diabetes medications offer unique mechanisms that affect appetite regulation and weight change. For instance, SGLT2 inhibitors and GLP-1 receptor agonists have shown potential in promoting weight loss in type 2 diabetes patients. This aspect can be beneficial for those struggling with obesity alongside diabetes. However, other medications, such as Sulfonylureas and Insulin, may lead to weight gain, making it crucial for healthcare providers to tailor treatment plans. Monitoring patient reactions to these medications is essential to optimize diabetes management. It may involve adjusting dosages or switching medications based on weight changes. Addressing weight gain or loss related to diabetes medications can impact overall health outcomes and treatment adherence. Conversations with healthcare professionals about these effects can empower patients to make informed choices regarding their diabetes management. Effectively managing weight alongside diabetes is not only beneficial for blood sugar control but can also enhance quality of life.
The body’s response to diabetes medications varies among individuals. Clinical research highlights that medications like Metformin are generally associated with minimal weight change, often promoting slight weight loss. This can be attributed to improvements in insulin sensitivity and appetite regulation. Conversely, patients using Insulin may experience increased appetite and subsequent weight gain as this medication acts to lower blood glucose levels by increasing insulin in the bloodstream. For those on SGLT2 inhibitors, studies indicate a favorable impact on body weight, likely due to increased glucose excretion. Moreover, GLP-1 receptor agonists not only enhance insulin secretion but can also lower appetite, leading to decreased caloric intake and weight loss. Understanding individual responses can aid in selecting the right diabetes treatment plan. Patients must engage actively in discussions with healthcare providers regarding their medication’s impact on weight. By doing so, adjustments can be made to ensure optimal control over their diabetes management. Overall, the relationship between diabetes medications, appetite, and weight illustrates the need for personalized treatment strategies.
Medication-related side effects are not limited to fluctuating weight; they can also include changes in appetite. Individuals taking certain diabetes medications might report increased hunger while others may experience a diminished desire to eat. This variance in appetite can complicate diabetes management, requiring ongoing evaluation. When a medication causes increased appetite and weight gain, it becomes a priority to discuss alternative options. Healthcare providers must monitor these changes closely in their patients, emphasizing the importance of regular follow-ups. The impact on appetite can also contribute to patients’ psychological wellbeing, leading to frustration or anxiety, particularly in those already managing diabetes. Therefore, maintaining an open line of communication about these side effects between patients and their healthcare teams is crucial. It allows for better management of weight and appetite concerns while adapting treatment plans. Addressing individual experiences with appetite and weight can improve medication adherence. Patients equipped with this knowledge can adopt healthier lifestyle choices, thus enhancing the efficacy of their diabetes treatment. Weight stability remains a pivotal goal in diabetes care, reinforcing the significance of personalized medication strategies.
Combining Lifestyle Changes with Medication
Alongside diabetes medications, lifestyle changes play a critical role in managing weight and appetite. Integrating dietary modifications, such as a balanced diet rich in whole foods, can complement pharmacological therapies. Regular physical activity is equally essential, as it helps regulate blood glucose levels and fosters weight management. Research indicates that patients who combine medication adherence with lifestyle changes often experience improved outcomes. For example, a Mediterranean diet focusing on fruits, vegetables, lean proteins, and whole grains can effectively support both diabetes control and healthy weight maintenance. Furthermore, portion control and mindful eating can enhance satiety and curb overeating, making it easier to manage appetite fluctuations. Healthcare providers often emphasize the synergy between medication and lifestyle strategies. This holistic approach not only targets diabetes management but also promotes overall health and wellbeing. It empowers patients to take ownership of their health journey, leading to more sustainable results. Patients are encouraged to work with dietitians and trainers to develop personalized plans tailored to their needs. The combined effect of these strategies can significantly enhance the quality of life for those living with diabetes.
Education about the various diabetes medications is vital to prevent weight-related issues. By understanding how each medication functions, patients can make informed decisions alongside their healthcare providers. Additionally, awareness can help detect side effects early, allowing for timely interventions. Some diabetes medications, especially those linked to weight gain, could necessitate trial and error to find the most suitable options. For instance, if a patient experiences unwanted weight gain while on Insulin, discussing alternatives like GLP-1 receptor agonists may be a viable solution. This proactive dialogue fosters a sense of empowerment among patients, enhancing their engagement in the treatment process. Furthermore, leveraging available resources, such as diabetes self-management education programs, can provide essential insights. These programs offer support systems where patients can share their experiences and strategies. Ultimately, education is crucial in promoting active participation in one’s own care. Knowledge about medication impacts can alleviate fears associated with diabetes management, paving the way for a healthier outlook. In summary, informed patients lead to better health outcomes, highlighting the importance of education in diabetes care.
The role of healthcare providers is indispensable in managing the impact of diabetes medications on weight and appetite. Continuous support and monitoring can make significant differences in patient outcomes. Regular check-ins allow healthcare teams to assess not only blood glucose levels but also weight fluctuations and appetite changes. Such comprehensive evaluations can facilitate timely treatment adjustments based on individual progress. Beyond medication management, professionals also provide vital lifestyle advice. Encouraging patients to adopt and maintain healthy habits is critical. Additionally, healthcare providers can help set realistic health goals that align with patients’ preferences. This collaborative approach fosters a supportive environment where patients feel encouraged to share their experiences. Furthermore, developing a strong patient-provider relationship enhances adherence to treatment plans. It promotes accountability and encourages patients to prioritize their health. With personalized guidance, patients can navigate the complexities of diabetes more effectively. Ultimately, the combination of effective communication, ongoing education, and support culminates in better overall management of diabetes. The focus on weight and appetite in the context of medication use illustrates the significance of a tailored approach to diabetes care.
In conclusion, diabetes medications have a multifaceted impact on weight and appetite, highlighting the importance of personalized care strategies. The relationship between medication effects and individual responses underscores the need for tailored treatment plans to meet patients’ unique needs. Moreover, integrating lifestyle changes with therapy is critical for optimizing outcomes. As healthcare providers and patients work together, they can navigate challenges and celebrate successes in diabetes management. By focusing on education and support, patients can better handle the complexities of their condition. This partnership not only improves adherence but also enhances the quality of life for individuals living with diabetes. Future advancements in diabetes medications and their formulations may further help minimize weight-related issues. Advancements may also contribute to more effective appetite control, a crucial aspect of overall diabetes management. Ongoing research continues to explore these dynamics, paving the way for innovative solutions. Ultimately, understanding medication impacts, fostering healthy habits, and maintaining effective communication can empower patients. Diabetes management is an evolving journey, yet strategic approaches can lead to positive health outcomes.