Diagnosing Endocrine Disorders: Tests and Procedures
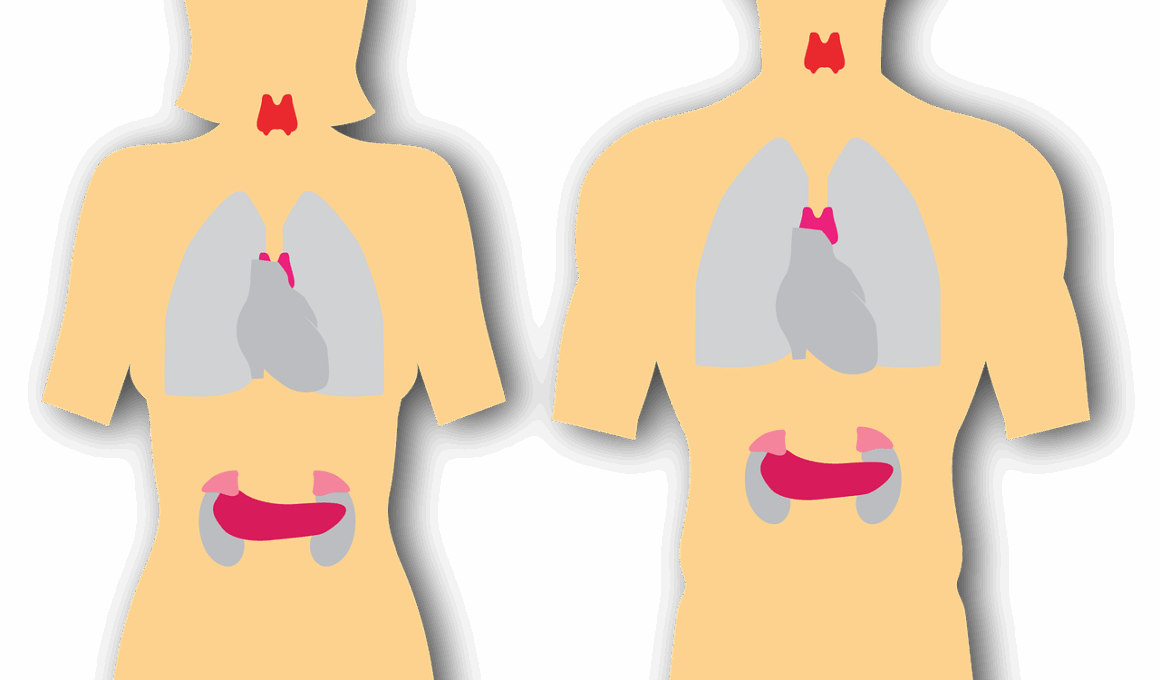
Endocrine disorders often require an accurate diagnosis through a series of tests and examinations. The endocrine system, which regulates hormones, plays a crucial role in body functions. To identify issues within this system, healthcare providers may suggest laboratory tests, imaging studies, and clinical evaluations. Common tests include blood tests to measure hormone levels, urine tests to check hormone excretion, and genetic testing in specific situations. Doctors utilize these methods to identify abnormalities or dysfunctions within various glands such as the pituitary, thyroid, adrenal, and pancreas. Symptoms that may warrant testing include unexplained weight changes, mood fluctuations, excessive thirst, or fatigue. Diagnosis often involves a thorough medical history, physical examination, and assessment of symptoms. To ensure the best outcomes, it is essential for patients to communicate openly with their healthcare providers about symptoms and concerns. Together, they can develop a targeted approach to diagnosis and management. Treatment options depend on the specific disorder diagnosed and may include hormonal therapies, lifestyle changes, or surgical interventions. A comprehensive evaluation allows for personalized care tailored to the needs of each patient.
The diagnostic process may involve different types of imaging studies, such as ultrasound, CT scans, or MRI. These imaging modalities provide detailed pictures of the glands, allowing for the identification of structural abnormalities. Also, the imaging results help distinguish between various types of endocrine disorders. For instance, an ultrasound may reveal thyroid nodules or adrenal tumors, prompting further investigation. The clarity provided by these imaging techniques is invaluable for precise diagnosis and treatment planning. Physicians also consider imaging studies alongside physical exams and laboratory results for a holistic understanding of a patient’s endocrine health. Moreover, these diagnostic procedures aid in monitoring the effectiveness of ongoing treatments. For example, after initiating therapy for thyroid disorders, follow-up imaging studies may evaluate any changes in structure or function. The collaboration between imaging specialists and endocrinologists plays a vital role in patient care. Additionally, advancements in technology continually improve imaging accuracy and reduce radiation exposure, enhancing overall patient safety and experience. In summary, various tests, including imaging studies, are instrumental in diagnosing and managing endocrine disorders effectively.
Laboratory Testing in Endocrinology
Laboratory testing is a cornerstone of diagnosing endocrine disorders, allowing healthcare providers to assess hormone levels in the body. Blood tests are commonly used in this context, as they measure specific hormone concentrations circulating in the bloodstream. For example, thyroid function tests evaluate levels of Thyroid Stimulating Hormone (TSH), T3, and T4, which are vital for determining thyroid health. Similarly, adrenal function may be assessed through cortisol tests or ACTH stimulation tests. Urine tests can also be used to measure hormone metabolites or levels, providing snapshots of endocrine function over time. These laboratory tests are often crucial in determining the presence of conditions such as diabetes, hyperthyroidism, or adrenal insufficiency. Patients may be asked to fast or follow specific instructions to ensure accurate results, with timing also playing a critical role in hormone testing. Moreover, repeat testing may be necessary for monitoring treatment responses or disease progression. Advances in laboratory technology continue to enhance the sensitivity and specificity of tests, enabling earlier detection of hormonal imbalances. Consequently, timely laboratory testing forms an integral part of comprehensive care in endocrinology.
Alongside blood and urine tests, genetic testing has become increasingly relevant in diagnosing endocrine disorders, particularly those with hereditary components. Genetic tests can help identify mutations associated with specific endocrine conditions, providing crucial information for management and family planning. For instance, conditions like Multiple Endocrine Neoplasia (MEN) syndromes or congenital adrenal hyperplasia may benefit from genetic screening to understand inheritance patterns and risks. The results from these tests aid clinicians in tailoring individualized treatment plans based on genetic predispositions and family histories. Genetic counseling may also be recommended to help patients comprehend the implications of test results fully. Additionally, early identification of genetic risks can inform proactive measures, potentially preventing or mitigating disease onset. This emphasizes the importance of genetic testing in not just diagnosis but also in long-term comprehensive care planning. Nevertheless, patients should engage in discussions with healthcare providers to understand the benefits and limitations of genetic testing. Emphasizing patient-centered care ensures that all aspects of hormonal health are addressed throughout the diagnostic process.
Symptom Assessment for Accurate Diagnosis
Accurate diagnosis of endocrine disorders often starts with a thorough symptom assessment conducted by healthcare professionals. Symptoms can vary widely depending on the specific glands involved and the hormonal imbalances present. For example, individuals with hypothyroidism may experience fatigue, weight gain, cold intolerance, or depression, prompting further testing and evaluation. In contrast, hyperthyroid patients might present with symptoms like anxiety, weight loss, and heat intolerance. The nuances in symptom presentation highlight the importance of careful patient history collection. Healthcare providers inquire about not only the presenting symptoms but also their duration, severity, and impact on daily life. Furthermore, a review of family medical history can uncover patterns or hereditary links to endocrine disorders. Additionally, lifestyle factors, such as stress levels, diet, and exercise, are key considerations. This comprehensive assessment aids in forming a complete clinical picture, guiding necessary conversations regarding lab tests and other diagnostic procedures. The emphasis on symptom assessment remains essential for effective communication between the patient and provider to establish trust and ensure that all symptoms are appropriately addressed.
Understanding the significance of symptom timing and variations goes hand in hand with accurate diagnoses. Hormonal fluctuations often lead to symptoms that may appear at different times or be influenced by various factors. For example, women may experience distinct hormonal changes during menstrual cycles, pregnancy, or menopause that can impact their well-being. Likewise, conditions like polycystic ovary syndrome (PCOS) can present with symptoms that fluctuate during a woman’s life stage. Recognizing the timing of symptoms can provide insight into underlying endocrine issues. Furthermore, endocrine disorders may present with symptoms that mimic other medical conditions, making it crucial for healthcare providers to distinguish these carefully. This process emphasizes the need for a multidisciplinary approach to diagnosis, which may involve endocrinologists, dieticians, and mental health professionals. By collaborating, they can offer patients comprehensive care and accurate diagnostic conclusions. This holistic approach supports better long-term health outcomes and empowers patients. Ultimately, recognizing and addressing the complexities of endocrine symptoms is foundational in achieving effective diagnosis and management.
Follow-Up and Long-Term Management
Follow-up care is essential after an initial diagnosis of endocrine disorders to monitor the effectiveness of the treatment plan. Ongoing assessments may involve repeat laboratory tests, imaging studies, and symptom evaluations tailored to individual needs. The frequency and complexity of follow-up appointments vary depending on the specific disorder diagnosed and the severity of symptoms presented. For instance, patients with diabetes may require regular monitoring of blood sugar levels and medication adjustments, while those with thyroid issues may have periodic hormone level checks. Moreover, these follow-ups help healthcare providers identify potential complications early, allowing for timely interventions. Patient education plays a critical role in long-term management, empowering them to recognize concerning symptoms or side effects that may arise during treatment. Regular follow-ups also foster better patient-provider communication, ensuring that patients can express their concerns and adapt the treatment plan as needed. The relationship established through consistent follow-ups contributes to positive health outcomes and enhances patient satisfaction. Consequently, ongoing management becomes a cornerstone of effective endocrine health, leading to a better quality of life.
The importance of lifestyle modifications cannot be overstated, as they significantly influence hormonal health and aid in managing endocrine disorders. Healthcare providers often recommend changes in diet, exercise, and stress management strategies as part of a comprehensive treatment plan. For example, individuals with diabetes benefit from balanced diets that balance carbohydrates and proteins, enhancing blood sugar control. Physical activity also plays a vital role in regulating hormones; regular exercise can improve insulin sensitivity and aid weight management. Moreover, stress-reduction techniques such as mindfulness, yoga, or counseling can have substantial impacts on hormonal balance. Patients who actively engage in lifestyle changes often report improved symptom management and overall well-being. This emphasizes the integral relationship between endocrine health and day-to-day living. Education about the connection between lifestyle factors and hormonal function is fundamental in empowering patients. By understanding how everyday choices affect their bodies, patients become more invested in their health journey. Ultimately, adopting a holistic approach that combines medical management with lifestyle modifications enhances patients’ long-term endocrine health and promotes a better quality of life.