How to Use Meal Timing to Support Blood Pressure Medication
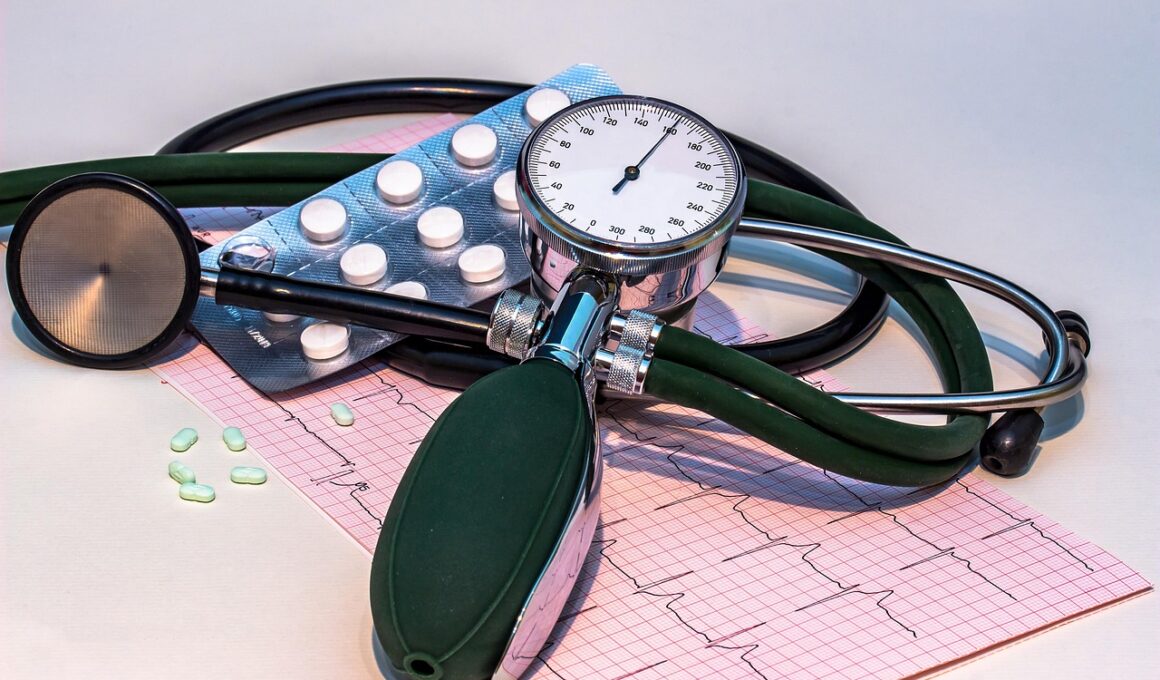
For managing blood pressure effectively, meal timing plays a critical role. Proper timing can enhance the effectiveness of blood pressure medications. It is essential to identify how food intake influences the absorption and efficacy of these medications. Meal timing can also affect the physiological responses of the body, including heart rate and blood flow. Observing a consistent meal schedule helps regulate blood sugar levels which in turn can influence blood pressure. This harmonization is vital for those taking medications for hypertension. The foods consumed and their timing can impact the medication’s effectiveness, thus adopting a schedule can promote better health outcomes. For example, it may benefit some individuals to take medications shortly before meals. Careful planning of when to eat can align with medication regimens to support overall health. Education on these practices is essential to help patients navigate meal timing effectively. By collaborating with healthcare providers, patients can develop personalized meal timing strategies that complement their hypertension management. Always consult with a healthcare professional before making changes to any dietary or medication plan to ensure safety and effectiveness.
The relationship between meal timing and blood pressure lies in how meals impact the body’s metabolic rate. When meals are consumed at regular intervals, it promotes optimal metabolism and better blood circulation. Inconsistent eating patterns or excessive snacking can lead to spikes in blood sugar and consequently affect blood pressure levels. Patients taking antihypertensive medications should be particularly mindful of their meal timing. Research indicates that regular meal times help maintain stable blood pressure levels throughout the day. Furthermore, specific dietary components combined with meal timing can lead to better management of blood pressure. For example, consuming a diet rich in whole grains, fruits, and vegetables, while being mindful of salt intake, can support blood pressure goals. Additionally, keeping track of food intake through meal journals helps patients recognize patterns between their diet and blood pressure readings. This analysis is essential in making informed decisions about meal timing and content. Patients should observe how their bodies respond to different meal timings and adjust accordingly. Consistent communication with healthcare providers about these observations can lead to improved outcomes and personalized dietary plans.
Optimal Timing for Meals
Identifying optimal times for meals can drastically improve blood pressure management. A regular eating schedule that includes three balanced meals daily can prevent fluctuations in blood pressure. Timing meals also aids in coordinating with medication schedules, ensuring that patients get the best possible outcomes. For example, taking medication after meals can enhance absorption, thus maximizing medication effectiveness. Furthermore, fasting for extended periods or relying solely on intermittent fasting may not be suitable for everyone, especially those with hypertension. Instead, focusing on balanced meals at consistent intervals offers a better approach. Incorporating healthy snacks can also help maintain energy levels without causing spikes in blood pressure. It is crucial to avoid large meals that might overload the digestive system, as this could lead to increased heart workload. Consuming smaller, nutritious meals can prevent such risks. Engaging in mindful eating practices during meals can also contribute to better overall health. Monitoring blood pressure before and after meals helps in understanding how food intake influences individual health. Keeping a detailed log of food and corresponding blood pressure readings can identify effective meal timings for each individual.
Incorporating time for hydration is another essential factor in meal timing and blood pressure control. Water intake before meals can assist digestion and help regulate blood pressure levels. It’s considered best practice to avoid consuming excessive amounts of caffeine and alcohol, particularly close to meal times, as both can lead to hydration issues and blood pressure spikes. Planning meals and drinks accordingly can help in maintaining optimal levels throughout the day. Additionally, it is advisable to consume electrolyte-rich foods, especially potassium, during meal times. Foods like green leafy vegetables, bananas, and legumes can support electrolyte balance. This balance is crucial for heart health and can aid in reducing blood pressure naturally. Moreover, having meals rich in omega-3 fatty acids, like fish and flaxseeds, can support overall cardiovascular health. By combining meal timing with proper hydration and healthy eating, individuals can enhance blood pressure management. Consulting with professionals regarding hydration strategies tailored to individual needs can optimize results and promote lasting habits for better health.
Monitoring and Adjusting Meal Timing
Monitoring the effects of meal timing on blood pressure can lead to more personalized management strategies. Keeping a detailed log of blood pressure readings alongside meal timing can shed light on effective methods that work. This practice allows patients to understand how specific meals at certain times influence their blood pressure levels. Regular follow-ups with healthcare providers can help fine-tune these strategies based on the data collected. Adjusting meal times based on blood pressure readings can significantly enhance the effectiveness of blood pressure medications. It is also essential to recognize patterns and trends in these data logs, as they can reveal which meal timings correlate with lower blood pressure. Additionally, experimenting with meal timing on weekends or days off can provide valuable insights into daily variations. Incorporating different foods and adjusting portion sizes aligned with timing might lead to improved outcomes. Accountability through meal tracking apps can encourage individuals to adhere to their plans. Combining these strategies ensures patients remain proactive about their health while effectively managing blood pressure and medication.
In summary, meal timing serves as a valuable tool for managing blood pressure alongside medication. Adopting a structured eating routine enhances medication adherence and overall health. Incorporating regular meal and snack times helps avoid spikes in blood pressure while ensuring optimal nutrient absorption from medications. Individuals should focus on balanced meals while being mindful of their dining schedule. Vigilance in keeping meal logs can show clear correlations, paving the way for personalized adjustments. Cooperating with healthcare professionals to develop and adjust meal timing plans tailored to individuals leads to improved health results. Every patient reacts differently to meal timings, so self-awareness becomes vital. Encouraging diverse food choices within the meal plan ensures all nutritional needs are met while supporting blood pressure goals. Furthermore, maintaining hydration and considering whole food options enrich the diet with essential nutrients. It’s crucial for individuals to stay informed through research and education on meal timing and hypertension. Overall, structured planning helps promote sustained lifestyle changes that will benefit long-term health outcomes and medication efficacy.
Conclusion: The Role of Meal Timing
In conclusion, meal timing significantly affects blood pressure management, especially for those on medications. By aligning eating schedules with prescribed medications, patients can enhance treatment effectiveness and achieve better results. Regular meals at consistent times maintain stable blood sugar levels and prevent fluctuations in blood pressure. Moreover, mindful eating practices and nutrient-rich foods contribute to better health. Understanding the linkage between food intake and medication helps foster a comprehensive approach to managing hypertension. Patients should continually communicate with healthcare providers for optimal advice tailored to their specific needs. The interplay of meal timing, dietary choices, and medication adherence creates a holistic approach essential for managing blood pressure safely. With the proper strategies, individuals can take charge of their health and significantly improve their quality of life while managing their blood pressure levels more effectively. Whether it’s experimenting with new meal timings, recording blood pressure fluctuations, or adjusting dietary habits, patients stand to gain from personalized plans that work best for them. Ultimately, a proactive approach to meal timing and medication will result in lasting health benefits and lower blood pressure.
In summary, meal timing serves as a valuable tool for managing blood pressure alongside medication. Adopting a structured eating routine enhances medication adherence and overall health. Incorporating regular meal and snack times helps avoid spikes in blood pressure while ensuring optimal nutrient absorption from medications. Individuals should focus on balanced meals while being mindful of their dining schedule. Vigilance in keeping meal logs can show clear correlations, paving the way for personalized adjustments. Cooperating with healthcare professionals to develop and adjust meal timing plans tailored to individuals leads to improved health results. Every patient reacts differently to meal timings, so self-awareness becomes vital. Encouraging diverse food choices within the meal plan ensures all nutritional needs are met while supporting blood pressure goals. Furthermore, maintaining hydration and considering whole food options enrich the diet with essential nutrients. It’s crucial for individuals to stay informed through research and education on meal timing and hypertension. Overall, structured planning helps promote sustained lifestyle changes that will benefit long-term health outcomes and medication efficacy.