The Relationship Between Fasting, Gut Microbiome, and Immune Function
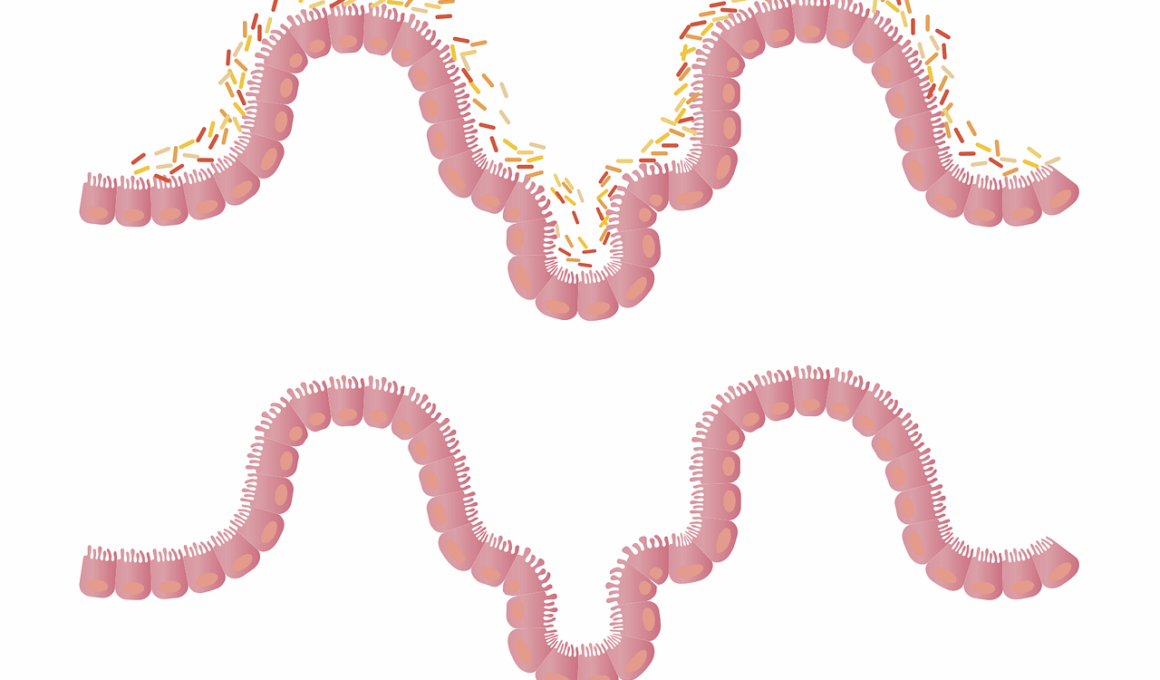
The gut microbiome is a complex ecosystem that plays a crucial role in our overall health. It comprises trillions of microorganisms, including bacteria, viruses, fungi, and other microbes. These organisms contribute to digestion, synthesis of vitamins, and modulation of the immune system. A healthy gut microbiome is linked to lower inflammation and better metabolic health. Recent research has shown that fasting influences this microbiome in profound ways. Intermittent fasting, for instance, can lead to shifts in microbial composition, promoting beneficial gut bacteria while reducing pathogens. By maintaining the balance of gut flora, fasting may enhance immune function. It may also work to inhibit the growth of bacteria known to cause disease. Moreover, fasting provides the gut with a much-needed break, allowing for repair and regeneration of the gut lining. This regeneration can support better digestion and absorption of nutrients. Investing time in understanding the relationship between fasting and gut health is essential for improving overall well-being. The implications for both physical and mental health are significant, opening pathways for therapeutic approaches targeting inflammatory diseases.
Fasting activates specific biological pathways that influence the gut microbiome’s composition and functionality. During fasting, the body undergoes metabolic changes that promote autophagy, a process that helps clean up damaged cells. This can lead to a more stable and diverse gut environment. Additionally, fasting has been shown to increase levels of short-chain fatty acids (SCFAs), which are beneficial for gut health. SCFAs are produced by gut bacteria from fermentable dietary fibers. They serve as a primary energy source for colon cells and have anti-inflammatory properties. This process may improve the gut barrier function, thereby preventing the entry of harmful substances into the bloodstream. A healthier gut barrier is beneficial for immune function, reducing the risk of various chronic diseases. When the gut microbiome thrives, it supports a robust immune response, assisting the body in resisting infections and inflammation. Moreover, fasting can modulate gut permeability, as it encourages a more balanced and beneficial microbiota. Understanding these complex interactions not only informs dietary choices but also advances our knowledge of gut health’s role in immunity and long-term health.
The Impact of Fasting on Inflammation and Immune Response
Fasting may significantly influence inflammatory processes and immune responses by altering gut microbiota. The reduction in caloric intake through fasting leads to metabolic adaptations that enhance the body’s ability to respond to inflammation. During fasting periods, the gut microbiome can shift toward a more beneficial composition, potentially lowering inflammatory markers. Particularly, beneficial bacteria can flourish, producing metabolites that inhibit the growth of harmful organisms. Interestingly, fasting can decrease the levels of pro-inflammatory cytokines, which are substances secreted by immune cells that promote inflammation. This moderation of immune responses contributes to a reduced risk for inflammatory diseases like arthritis and chronic gastrointestinal disorders. Fasting also enables the phenotypic transition of immune cells, fostering a more regulatory type of immunity. This change assists the body in reducing unnecessary inflammatory responses that contribute to autoimmune diseases. As research continues to unveil these connections, understanding specific fasting protocols tailored to individual needs could become a critical component of dietary interventions aimed at optimizing gut health and immune function. Further studies will enhance our comprehension of the potential mechanisms involved.
Dietary patterns play a significant role in cultivating a healthy gut microbiome. However, fasting as an interventional strategy can prove even more advantageous in fortifying gut health. Various fasting protocols have different effects on the microbiome, highlighting the necessity to choose an appropriate method. One popular approach is the 16:8 method, which involves an eight-hour eating window followed by a sixteen-hour fast. This method appears to promote beneficial bacterial strains that support gut health while providing adequate time for the gut to reset. Another method, alternate-day fasting, gives the gut a significant break from processing food, allowing diverse microbiota to flourish. Both methods can enhance metabolic health, manage weight, and reduce inflammation, leading to improved immune function overall. Emphasizing the importance of a balanced diet rich in anti-inflammatory foods during eating windows can further optimize these benefits. Dietary fiber is particularly important, as it serves as food for beneficial gut bacteria, ensuring their growth and activity. Incorporating a mix of fruits, vegetables, whole grains and fermented foods enhances microbiome diversity to provide maximum immune-supporting benefits.
Fasting and Its Effects on Gut Bacteria Diversity
Diversity in gut bacteria is essential for optimal health. A diverse microbiome is better able to adapt to challenges such as infections and dietary changes. Fasting can promote microbial diversity by allowing various beneficial bacteria to thrive while suppressing harmful strains. Research indicates that fasting promotes the growth of bacteria that produce SCFAs, such as acetate and butyrate, found mostly in healthy gut microbiomes. In turn, these SCFAs provide energy for colonic cells and help regulate the immune system. Additionally, fasting can trigger a phenomenon known as ‘microbiome resilience,’ wherein the microbiome can recover quickly from disturbances. This capability is essential in maintaining overall gut homeostasis. It emphasizes the importance of avoiding constant eating practices that lead to an unbalanced microbiome. Furthermore, the timing of these fasting periods can also significantly impact which bacteria become dominant in the gut. Studies have shown that aligning fasting windows with circadian rhythms may optimize gut health. To maximize those benefits, it’s advisable to consider individualized fasting strategies that suit one’s lifestyle while focusing on overall balanced nutrient intake.
In conclusion, understanding the profound relationship between fasting, gut microbiota, and immune function underscores the significance of dietary choices for health. The connections revealed in various studies create an opportunity for incorporating fasting into healthcare recommendations aimed at improving public health. Implementing fasting protocols could mitigate the rise of lifestyle-related diseases, enhancing the quality of life for many individuals. As research evolves, so too should our awareness of how we can utilize dietary interventions as tools for health promotion. Future studies should explore different fasting regimens more thoroughly and investigate their long-term impacts on gut health and immune function. Such progress is critical to establishing guidelines for practitioners working in nutrition, health, and wellness space. It’s imperative to educate the public on the benefits of fasting and its comprehensive effects on gut health. Ultimately, a healthy gut microbiome is integral to a well-functioning immune system. By prioritizing both healthy eating and fasting, we can achieve robust gut health alongside fortified immune responses, promoting overall vitality. The journey towards understanding our bodies continues, and fasting stands as a valuable key in maintaining our health.
To summarize, embracing fasting as a fundamental aspect of well-being can yield numerous benefits, particularly for gut microbiota and the immune system. As we uncover deeper insights into the functioning of our microbiome, it becomes evident that lifestyle choices, especially dietary ones, play pivotal roles in shaping our health landscape. Understanding the intricate dialogues between our diets, microbiome composition, and immune function offers invaluable strategies for disease prevention and health promotion. Embracing such knowledge empowers individuals to take control of their health, prioritizing practices that enhance both gut health and immune resilience. Fasting not only bridges the gap between diet and immunity but also opens new paradigms in personal health management. As research continues to illuminate the health transformations achievable through fasting, individuals are encouraged to experiment with different fasting methods. Consulting healthcare professionals to tailor fasting approaches aligned with specific health goals will be crucial. By promoting this holistic understanding of diet and its multifaceted connections to health, we can inspire greater awareness and encourage smarter dietary approaches across diverse populations.