Effects of Psychological Stress on Gut Microbiota Composition
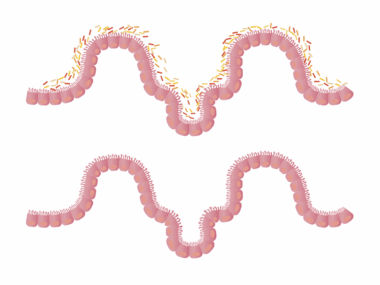
The human gut microbiota is a complex community of microorganisms that plays a crucial role in gut health and overall well-being. Recent studies have shown that psychological stress can significantly impact gut microbiota composition. Stress triggers various physiological responses, including hormonal changes that influence gut health. These responses can lead to dysbiosis, an imbalance in microbial populations, resulting in health issues. Factors contributing to this imbalance include diet, lifestyle, and genetics, but stress is a significant modulator. Stress-induced changes may result in the overgrowth of harmful bacteria while suppressing beneficial strains. This alteration of gut flora can affect digestion and immune function. Moreover, it has been linked to various gastrointestinal disorders, such as irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD). Understanding the relationship between stress and gut microbiota is essential for developing potential treatments that could restore balance. Some studies suggest that managing stress through lifestyle changes or psychological therapies might positively influence gut health, contributing to the stabilization of healthy microbiota. Thus, addressing psychological stress could be crucial in maintaining a healthy gut. This area warrants further investigation in clinical research.
The gut-brain axis forms a critical link between psychological stress and gut microbiota. The bidirectional communication between the brain and the gut is mediated through neural, hormonal, and immunological pathways, demonstrating that mental health significantly impacts gastrointestinal health. Stress affects this axis through the hypothalamic-pituitary-adrenal (HPA) axis, resulting in the release of cortisol and other stress hormones. Elevated cortisol levels can lead to the alteration of gut microbial diversity, impacting beneficial bacteria such as Bifidobacterium and Lactobacillus. The gut-brain axis suggests that psychological stressors can lead to gastrointestinal symptoms, further exacerbating stress levels in individuals. This cyclical relationship indicates that tackling psychological stress could, in turn, improve gut health. Moreover, ongoing research is identifying the potential for probiotics and prebiotics as effective interventions, aiming to restore microbial balance during stress. Incorporating dietary modifications, including fiber-rich foods, may foster beneficial microbial growth that counters the negative effects of stress. These strategies underscore the importance of considering both psychological and gut health in a holistic treatment framework to improve overall quality of life and health outcomes.
Stress can exacerbate gut issues, revealing a strong connection between mental health and gastrointestinal function. Dysbiosis increases the risk of developing conditions such as anxiety and depression, creating a cycle that affects both psychological and gut health. Individuals experiencing chronic stress often report digestive symptoms like bloating, abdominal pain, and irregular bowel movements. Stress management techniques, including mindfulness and cognitive-behavioral therapy (CBT), have shown promise in alleviating both psychological and gastrointestinal symptoms. Evidence suggests that these techniques can help restore balance in gut microbiota, improving overall gut health. Incorporating regular exercise, sufficient sleep, and healthy nutrition into daily routines also mitigate the effects of stress on gut microbiota. For instance, fermented foods rich in probiotics can support the growth of beneficial bacteria, while reducing the intake of processed foods may decrease inflammation and dysbiosis. A psychosomatic approach is warranted, allowing practitioners to consider stress-related symptoms in the context of gut health. Addressing both the physical and mental components of health can lead to comprehensive treatment strategies. Therefore, understanding the interplay between psychological stress and gut microbiota composition is vital for optimal health.
The Role of Diet in Modulating Gut Microbiota During Stress
Diet plays a crucial role in influencing gut microbiota composition, particularly under stress. Nutrient-rich foods, including fruits, vegetables, whole grains, and fermented foods, support a diverse and thriving gut microbiome. However, stressful situations often lead individuals to opt for unhealthy comfort foods, which can negatively impact gut health. High-fat, high-sugar diets are linked to reduced microbial diversity and increased inflammation. These dietary patterns can exacerbate stress effects on gut health. Studies indicate that specific dietary choices can mitigate stress’s negative impact on gut microbiota. For instance, diets rich in omega-3 fatty acids have been associated with beneficial changes in gut composition and reduced inflammation. Furthermore, fiber intake encourages the growth of beneficial microorganisms, which helps maintain a balanced gut. The Mediterranean diet, renowned for its emphasis on whole foods, has demonstrated positive effects on gut microbiome stability. Implementing dietary changes alongside stress management strategies could yield synergistic benefits. Nutrition education should emphasize the importance of gut health, especially in populations experiencing high levels of stress. This holistic approach can empower individuals to make healthier food choices that support both mental and gut health.
Probiotics emerge as a promising intervention for restoring gut microbiota balance during stressful periods. These live microorganisms confer health benefits by influencing the gut microbiome positively. Several studies have examined the efficacy of probiotics in alleviating stress-related digestive symptoms. For example, specific strains like Lactobacillus and Bifidobacterium are known to enhance gut health and modulate the body’s stress response. Clinical evidence suggests that probiotics can help reduce stress and anxiety levels, partly due to their ability to influence the gut-brain axis. Incorporating probiotic-rich foods such as yogurt and kefir into one’s diet may enhance gut health and improve psychological well-being. Additionally, prebiotics, which feed beneficial bacteria, serve as an important adjunct to probiotics, promoting their efficacy. A combination of both probiotics and prebiotics can create a symbiotic effect, providing comprehensive support. Alongside dietary interventions, ongoing psychological support is crucial in managing stress levels effectively. The integration of probiotics into clinical practice offers a novel approach to addressing gut health while considering the psychological factors involved. Further research is vital to establish optimal strains and dosages for stress reduction and overall gut wellness.
Conclusion: The Interconnection of Psychological Stress and Gut Health
Understanding the effects of psychological stress on gut microbiota composition is essential for fostering better health outcomes. The interplay between mental health and gut health reveals a complex relationship that highlights the need for integrated treatment approaches. By addressing both psychological factors and gut microbiota composition, healthcare professionals can offer a holistic perspective. It is imperative to recognize that neglecting one aspect can hinder improvement in the other. Stress management practices, including mindfulness, nutrition, and lifestyle modifications, play a vital role in promoting a balanced gut microbiome. By fostering beneficial bacteria through dietary choices and considering psychological interventions, individuals can take proactive steps toward enhancing their overall health. The implications of ongoing research will help identify effective strategies to manage stress and restore gut health. Furthermore, collaboration between mental health and nutrition professionals could lead to innovative therapies that leverage the gut-brain axis. Achieving optimal gut health involves recognizing its influence on emotional well-being and vice versa. This interconnection necessitates ongoing exploration and understanding of the dynamic relationship between psychological stress and the gut microbiome for improved public health.
In summary, the effects of psychological stress on gut microbiota composition are profound, impacting both physical and mental health. The gut’s intricate balance is vulnerable to the fluctuations caused by stress, revealing the importance of maintaining a healthy lifestyle. Managing stress through adequate support systems and lifestyle adjustments, combined with nutrition and probiotic interventions, can enhance gut health and improve quality of life. An integrated approach that considers the multifaceted nature of health, encompassing psychological, dietary, and lifestyle factors, is crucial for effective treatment. Educating individuals on the importance of the gut microbiome and its relationship with stress can empower them to make informed choices. This research area is continually evolving, and ongoing studies will shed light on effective practices for maintaining gut health amidst everyday stressors. As we continue to explore the gut-brain connection, novel insights will emerge, potentially leading to breakthroughs in treatment. Public awareness regarding the significance of gut health should be emphasized in health promotion efforts. Ultimately, a comprehensive understanding of psychological stress’s impact on gut microbiota is key to advancing holistic health initiatives.
By exploring the bi-directional relationship between psychological stress and gut microbiota, we can establish better health practices that incorporate stress management and nutritional interventions. Future research must focus on how specific stressors uniquely influence gut health and identify personalized strategies to alleviate distress. Additionally, interventions targeting lifestyle changes may prove beneficial in rebalancing gut microbiota amidst stress. Public health messages should reinforce the importance of recognizing the signs of stress and its repercussions on health, paving the way for preventive measures. Approaches that integrate mental health care with nutritional guidance could empower individuals to take proactive steps towards improving their well-being. With a deeper understanding of the intersection between mental health and gut microbiome, we can promote healthier lifestyles. Studies exploring the effects of supplements, such as omega-3 fatty acids and various probiotics, can provide valuable insights. Ultimately, researchers and healthcare providers should collaborate to create a better understanding of the gut’s role in overall health, specifically concerning the impact of psychological stress. This alignment of knowledge and practice can ultimately enhance the quality of healthcare and contribute to reducing the prevalence of stress-related health issues.