The Relationship Between Gut Microbiome and Hypoglycemia in Diabetes
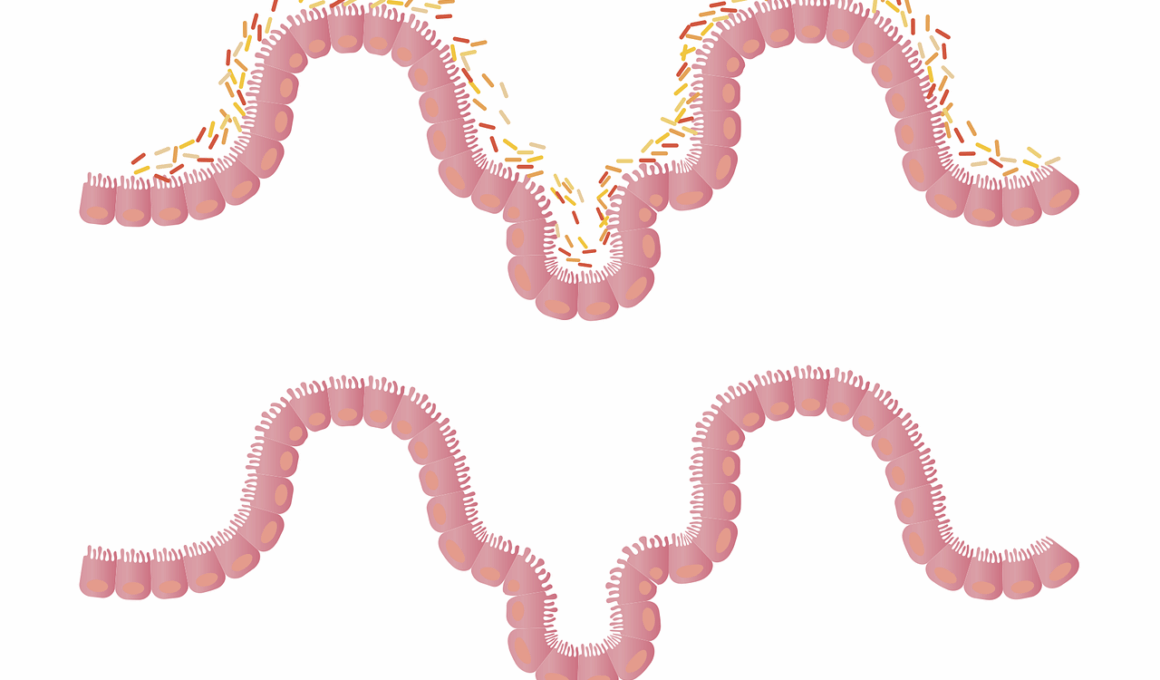
The gut microbiome plays a significant role in metabolic processes, including glucose metabolism. Research suggests that a diverse gut microbiome can positively influence insulin sensitivity, reducing the risk of diabetes and hypoglycemia. In diabetic patients, the balance of gut bacteria can become disrupted, leading to changes in how the body processes carbohydrates. A healthy microbiome can help regulate blood sugar levels and curb episodes of hypoglycemia. It achieves this by fermenting dietary fibers, producing short-chain fatty acids, and enhancing gut barrier function. Additionally, certain bacteria have been implicated in modulating inflammation, which is crucial for maintaining insulin sensitivity. Transferring beneficial microbes into the gut has shown promising results in animal models, demonstrating a protective effect against hypoglycemia. These findings underscore the potential of probiotics and prebiotics in diabetes management. Nutritional strategies focusing on fiber-rich foods can aid in replenishing healthy gut bacteria. Therefore, understanding the intricate relationship between our gut health and glucose levels could pave the way for innovative dietary interventions for diabetes patients.
Hypoglycemia is characterized by abnormally low blood sugar levels, leading to symptoms like weakness, confusion, and sweating. In diabetes, hypoglycemia can be a serious concern, particularly for patients on insulin therapy. Studies indicate that an imbalance in the gut microbiome may exacerbate hypoglycemic events by hindering the body’s ability to maintain glucose homeostasis. Factors such as diet and antibiotic use can disrupt gut bacteria diversity, contributing to glucose regulation issues. For instance, Western diets high in fat and sugar have been associated with decreased microbial diversity, which correlates with insulin resistance. Conversely, diets enriched with fibrous vegetables and fermented foods promote healthy gut flora. Maintaining a balanced gut microbiome may therefore offer a protective layer against hypoglycemia. Probiotics, found in fermented foods like yogurt and sauerkraut, can introduce beneficial bacteria that aid digestion. But the key is sustainability: integrating these foods into a daily routine promotes long-term gut health, thereby potentially stabilizing blood glucose levels. By focusing on nutrition, patients may lessen their risks of hypoglycemic episodes, thereby improving overall management of diabetes.
Research has also highlighted the link between gut microbes and hormonal regulation, particularly hormones involved in glucose metabolism. Hormones such as GLP-1 (glucagon-like peptide-1) are crucial for stimulating insulin secretion and moderating blood sugar levels. Certain gut bacteria can influence the secretion of GLP-1, thus impacting the body’s response to glucose intake. High levels of a specific group of bacteria have been found to increase GLP-1 levels, leading to better blood sugar control and fewer occurrences of hypoglycemia. Moreover, the health of the gut microbiome can also affect levels of other hormones like ghrelin, which can stave off feelings of hunger, thus assisting with caloric intake and management. This creates a feedback loop where a healthy microbiome fosters better glucose regulation. Additionally, those undergoing treatment for diabetes might benefit from supplements aimed at restoring gut health. Foods that nourish beneficial bacteria can serve as an excellent complement to diabetes medications, enhancing their efficacy. Thus, ongoing research aims to fully elucidate the mechanisms behind these interactions to unlock new therapeutic avenues.
Implications for Dietary Interventions
The implications of gut microbiome research extend to dietary interventions aimed at diabetes management. Incorporating foods rich in soluble fiber can enhance gut health, improve bacterial diversity, and, consequently, stabilize blood glucose levels. Foods like legumes, oats, and whole grains are excellent sources of soluble fiber. These fibers are fermented by gut bacteria, resulting in the production of short-chain fatty acids that exert beneficial effects on metabolism. Emphasizing a diet that encourages the growth of beneficial microbes through prebiotics is vital. Prebiotics, such as inulin and oligofructose, can significantly increase the number of beneficial bacteria in the gut. The synergistic effect of probiotics and these prebiotics can create a more favorable environment for gut health. Furthermore, tracking dietary patterns and individual responses to different foods can aid in customizing diets specific to a diabetic person’s needs. Therefore, nutritionists and healthcare providers should collaborate to create tailored dietary plans. This personalized approach could drastically reduce the frequency of hypoglycemic events, enhancing overall diabetes management and improving quality of life.
In clinical settings, understanding the gut microbiome’s role in diabetes could transform treatment protocols. By integrating microbiome analysis into routine diabetes care, healthcare providers can better assess individual risks for hypoglycemic events. This analysis can also reveal specific bacterial imbalances that may need addressing. For instance, performing stool tests might help identify low levels of critical beneficial bacteria often tied to glucose regulation. Additionally, educating patients about their gut health is crucial for empowering them in their diabetes management journey. Knowledge about how diet can influence gut microflora can motivate behavior changes that promote better health outcomes. Furthermore, future research could lead to personalized probiotics tailored to restore specific gut microbial profiles for diabetes patients. Clinical trials are ongoing to test the efficacy of such targeted therapies. Comprehensive strategies that include nutritional management, lifestyle changes, and potential probiotic use could lead to more effective hypoglycemia prevention. Such preventative measures might not only enhance the well-being of diabetic patients but also reduce healthcare costs significantly by minimizing complications associated with hypoglycemia.
The relationship between the gut microbiome and systemic health emphasizes the importance of maintaining a balanced diet. This balance is critical for diabetic individuals who are at risk for hypoglycemia. Health professionals should prioritize educating patients on the importance of dietary diversity, focusing on foods that promote a proliferative environment for beneficial bacteria. Foods rich in vitamins, minerals, and antioxidants are particularly beneficial for overall health and maintaining a balanced microbiome. Furthermore, understanding the effects of environmental factors, such as stress and sleep, can help individuals address the holistic aspects of health. Chronic stress and poor sleep often disrupt metabolic processes, further complicating diabetes management. Teaching patients about stress-reducing techniques and the importance of restorative sleep can play a vital role in their overall health strategy. The synergy of a healthy diet, good sleep hygiene, and effective stress management creates a comprehensive health plan. Such strategies empower individuals to take charge of their gut health, ultimately improving their diabetes management and reducing incidents of hypoglycemia. Continued education and research in this area will provide exciting prospects for treating diabetes.
Conclusion: Future Directions
In conclusion, the gut microbiome significantly influences the management of diabetes and episodes of hypoglycemia. Further research is needed to uncover the complex interactions between various gut bacteria and metabolic processes. Future studies should delve into the specific types of microbiota that confer health benefits for diabetic individuals. With the growing interest in personalized medicine, there lies potential for developing tailored dietary recommendations and probiotic supplements. Monitoring gut health could become a standard part of diabetes management, providing a comprehensive approach to treatment. Enhanced understanding could enable healthcare providers to design effective interventions aimed at stabilizing blood glucose levels in a safe and sustainable way. Moreover, as technology evolves, integrating microbiome analysis into personalized healthcare could reshape treatment pathways. The future of diabetes management is not just limited to pharmaceuticals but extends to embracing gut health and nutrition as pivotal components of care. Ultimately, a multi-faceted approach that includes dietary management, gut health maintenance, and lifestyle modifications could lead to lasting improvements in the lives of individuals living with diabetes.