The Link Between Tobacco Use and Diabetic Foot Ulcers
The connection between tobacco use and diabetic foot ulcers is a critical aspect of managing diabetes. Smoking poses numerous health risks, particularly for those living with diabetes. Studies indicate that smoking contributes significantly to the prevalence of foot ulcers among diabetic individuals. It does this by impairing blood flow and reducing oxygen transport to various tissues, which are vital processes for healing. Chronic wounds, especially foot ulcers, often occur in diabetic patients due to reduced circulation. Furthermore, smoking presents additional challenges, complicating the usual management of diabetes. For many, the lifestyle changes required for better blood sugar control are hindered by nicotine dependence. Smoking affects blood sugar levels directly, leading to spikes that can exacerbate diabetes complications. This results in a vicious cycle of worsening health outcomes. Patients need to understand these linking factors to make informed choices about their health. Awareness can motivate smokers with diabetes to seek cessation programs that provide support. Quitting smoking leads to improved circulation, better healing rates, and overall enhanced well-being. Such improvements can significantly impact the management of diabetes and the risk of developing serious complications.
Impact of Smoking on Wound Healing
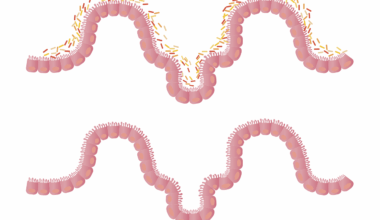
Smoking has a profound impact on the body’s ability to heal, particularly for those with diabetes. Nicotine and other harmful substances in tobacco reduce blood flow to the skin and other tissues. As a result, any existing wounds, particularly diabetic foot ulcers, may heal at a much slower rate. This delayed healing is attributed to a decrease in the availability of essential nutrients and oxygen, both crucial for repair processes. Additionally, smoking increases the risk of infection, further complicating wound healing. Infections can delay recovery and lead to more severe outcomes, including the possibility of amputation, which is a genuine concern for individuals with diabetes. The inflammatory response is also heightened in smokers, leading to increased tissue damage. This comprehensive understanding emphasizes the need for smokers with diabetes to quit to optimize their health outcomes. Furthermore, healthcare providers play a crucial role in this regard. They should routinely discuss these risks, providing resources and support for cessation. Ultimately, the goal is to enhance wound healing and reduce overall complications from diabetes, leading to a healthier life for those impacted.
The impact of smoking on diabetes extends to complications beyond just foot ulcers. It is important to recognize how this harmful habit can exacerbate numerous issues faced by diabetic patients. For instance, smoking contributes to cardiovascular diseases, which are prevalent among diabetics. The cardiovascular system is already compromised in diabetes, making it crucial to avoid any additional stressors. Patients who smoke are at a significantly higher risk of heart attacks and strokes. Additionally, smoking is associated with reduced insulin sensitivity, which complicates blood sugar management. This contributes to higher glucose levels that can lead to further complications over time. Educating patients on the full scope of risks they face can motivate them to consider quitting. Healthcare professionals should provide a comprehensive overview of the ways smoking can drastically affect their health. Incorporating smoking cessation discussions into regular diabetes management sessions can yield positive results. These interactions allow for the delivery of tailored resources and support that encourages positive lifestyle changes. Engaging patients in this manner is essential, as enhancing their understanding directly correlates with success in their cessation efforts.
Prevention Strategies
Preventing diabetic foot ulcers in smokers requires comprehensive strategies focused on lifestyle modification. Smoking cessation is the most critical step toward improving overall health for diabetic patients. Health professionals must assist patients in developing personalized cessation plans. This approach should be multifaceted, addressing psychological factors, providing nicotine replacement therapies, and offering various supportive resources. Regular follow-up appointments can help reinforce the importance of adherence to the cessation plan and allow for adjustments based on individual progress. In parallel, effective foot care education is paramount for those living with diabetes. Patients should be taught about proper footwear choices and daily foot inspections to identify any signs of issues early. Also, maintaining consistent blood sugar levels can significantly reduce ulcer risk. Incorporating educational workshops can empower patients to take charge of their health. Group settings provide peer support and share success stories, enhancing motivation and commitment to lifestyle changes. Furthermore, collaboration with dietitians may aid in developing healthy meal plans that improve blood sugar control while simultaneously addressing nicotine cravings. This holistic approach plays a vital role in preventing complications and fostering a healthier lifestyle overall.
In addition to individual strategies, community programs can significantly enhance cessation efforts for smokers with diabetes. Accessible community resources foster an environment of support, facilitating lifestyle changes that are essential for managing diabetes effectively. Local organizations and healthcare facilities can work together to create programs focused on education about the intersections between smoking and diabetes. Offering workshops, seminars, and support groups not only raises awareness but also provides the tools needed for quitting smoking. These groups can serve as safe spaces for sharing experiences and challenges, allowing participants to learn from one another. Collaboration with local pharmacists can enhance access to nicotine replacement therapy and educational materials. Additionally, community health workers can play an important role in outreach initiatives to inform individuals about both diabetes management and smoking cessation. Engaging more people in this critical conversation can lead to a greater collective understanding of health risks. This holistic approach fosters a culture of prevention and awareness, benefiting all members of the community. Enhancing community engagement can significantly reduce obesity, smoking rates, and the prevalence of diabetes-related complications.
Emotional and Psychological Aspects
Addressing the emotional and psychological factors associated with smoking and diabetes is imperative for successful management. Many diabetics find comfort in smoking, believing it alleviates stress. However, this reliance on cigarettes can hinder their ability to cope with diabetes effectively. Understanding the reasons behind smoking habits can help healthcare providers tailor cessation strategies. For example, stress management techniques, such as mindfulness and relaxation exercises, can replace smoking as a coping mechanism. Establishing support networks that include mental health professionals can empower patients to confront their emotional triggers. These professionals can provide counseling to develop healthier coping strategies while navigating the complexities of living with a chronic illness. Furthermore, incorporating mental health screenings into standard diabetes care can reveal underlying psychological concerns that may fuel smoking habits. Patients may not consider seeking help for these issues, so proactive discussions can open important dialogue. Combining emotional support with the right medical assistance can lead to positive health outcomes. Stronger mental health contributes to a more robust resolve to quit smoking. Ultimately, focusing on all aspects of health will result in enhanced quality of life for diabetic patients.
As diabetic cases continue to rise globally, understanding the interplay between smoking and diabetes becomes increasingly essential. Public health initiatives should focus on raising awareness about the risks of smoking for those with diabetes. Comprehensive educational campaigns could empower individuals to reduce smoking rates, enhancing public health outcomes. These campaigns can focus on distributing information through various media outlets, highlighting the dire consequences of smoking on diabetes management. Partnerships with local organizations can amplify their reach, providing community-based approaches to education and prevention. Furthermore, incorporating tobacco use assessments into routine diabetes screenings can help identify at-risk patients early. By addressing smoking during consultations, healthcare providers can help minimize the associated risks of complications. This proactive approach in tackling smoking may significantly improve both diabetes management and overall health. Collaboration between healthcare providers, educators, and community members plays a key role in these efforts. Creating targeted programs can effectively educate at-risk populations and positively influence lifestyle changes. The fight against diabetes-related complications is a shared responsibility that can dramatically improve public health.
Conclusion
In conclusion, the link between tobacco use and diabetic foot ulcers presents a significant challenge to effective diabetes management. Recognizing this critical relationship is vital for patients and healthcare providers alike. Smoking contributes to many health complications for individuals with diabetes and directly influences the risk of foot ulcers. Through comprehensive education, support, and preventative strategies, we can promote healthier lifestyles for diabetics. Encouraging tobacco cessation must be prioritized to enhance healing, improve circulation, and ultimately improve quality of life. Additionally, mental health support plays a significant role in successful smoking cessation efforts. Patients must have access to a myriad of resources to aid in this journey. By fostering essential collaborations among healthcare professionals, community organizations, and support networks, we can better equip individuals to make informed choices. Addressing this vital issue means creating a future of improved health outcomes for those struggling with diabetes. This focus can drastically reduce the incidence of foot ulcers and other complications linked to tobacco use. The resulting positive behaviors will foster a healthier society, ultimately leading to thriving communities.