Probiotics and Their Impact on Inflammatory Bowel Disease
Inflammatory Bowel Disease (IBD) is a term that encompasses chronic inflammatory conditions of the gastrointestinal tract, including Crohn’s disease and ulcerative colitis. Probiotics are live microorganisms that, when administered in adequate amounts, can confer a health benefit on the host. The balance of gut bacteria is crucial for maintaining gut health, and probiotics can help to restore this balance. Emerging research indicates that probiotics may modulate inflammatory responses, strengthen the gut barrier, and improve gut microbiota composition. Their effectiveness in managing IBD is linked to reducing symptoms, promoting remission, and possibly even influencing the disease’s course. Several strains of probiotics, such as Lactobacillus and Bifidobacterium, have garnered attention for their positive effects in clinical settings. However, more extensive and well-structured clinical trials are necessary to determine the most effective strains and dosages for individuals with IBD. Those suffering from this condition must consult healthcare professionals to tailor probiotic usage to their specific needs, combining dietary and lifestyle modifications for optimal gut health. Probiotics could represent a valuable addition to conventional treatments for IBD, improving patients’ quality of life.
The Role of Gut Microbiome in IBD
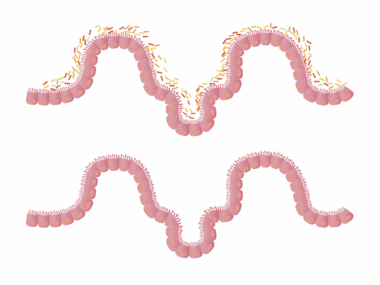
The gut microbiome consists of trillions of microorganisms, including bacteria, viruses, and fungi, that inhabit our intestines. This complex ecosystem plays a vital role in maintaining gut health and overall well-being. In individuals with Inflammatory Bowel Disease (IBD), the composition of the gut microbiome is often altered, which may contribute to inflammation and disease exacerbation. A rich and diverse gut microbiome is essential for immune system regulation. Research suggests that dysbiosis, or microbial imbalance, can promote the onset and persistence of IBD. Probiotics can help restore this balance by reintroducing beneficial bacteria into the gut. These microorganisms compete with harmful bacteria for resources and also produce substances that inhibit pathogen growth, thereby reducing inflammation. Studies indicate that certain probiotic strains may also enhance mucosal healing and promote remission in IBD patients. However, the specific mechanisms through which probiotics exert their beneficial effects in IBD require further exploration. A comprehensive understanding of the interaction between probiotics and the gut microbiome can facilitate the development of targeted therapies for individuals suffering from this complex condition.
Research on the use of probiotics in IBD has produced encouraging results, but there remains a degree of skepticism within the medical community regarding their efficacy. Some studies have shown that specific probiotic strains can lead to significant improvements in symptom severity and frequency of relapses. In particular, the strain Saccharomyces boulardii has been demonstrated to reduce diarrhea and improve quality of life for patients with IBD. However, inconsistencies in study results also highlight the need for additional clinical trials. Variability in the probiotics’ formulation, dosage, and duration of treatment complicates the ability to make broad recommendations. Moreover, individual responses to probiotics can vary considerably, suggesting that personalized approaches are necessary. It is essential to consult healthcare professionals to determine the appropriate probiotic strains and dosages that might benefit individuals with different types of IBD. Despite these challenges, the potential for probiotics to act as adjunctive therapies alongside traditional medical treatments remains an exciting area of exploration. As researchers continue to unravel the complexities of the gut microbiome and its impact on IBD, future therapies may become more effective and targeted.
Selecting the Right Probiotic for IBD
Choosing the correct probiotic strain is crucial for individuals with Inflammatory Bowel Disease (IBD), as not all probiotics provide the same benefits. The selection process should consider various factors, including the specific type of IBD, the individual’s symptoms, and their overall health profile. Notably, certain probiotic strains, such as Lactobacillus rhamnosus and Bifidobacterium infantis, have shown promise in clinical trials for managing IBD symptoms. The dosage and duration of probiotic therapy also significantly influence outcomes. In addition to strain specificity, it is important to choose high-quality probiotics, ensuring they contain viable organisms and meet specific health standards and guidelines. Individuals should also pay attention to the form of probiotics available, which may range from capsules and powders to fermented foods. Incorporating probiotic-rich foods like yogurt, kefir, and sauerkraut into the diet may additionally benefit gut health. It is vital to work closely with a healthcare provider when integrating probiotics into the treatment plan. These professionals can help monitor progress and make necessary adjustments, ensuring safe and effective management of IBD symptoms.
While probiotics offer potential benefits for individuals with Inflammatory Bowel Disease (IBD), lifestyle factors also play a significant role in gut health. A diet rich in fiber, whole grains, fruits, and vegetables can support the growth of beneficial gut bacteria. Conversely, processed foods and excessive sugar may negatively affect the gut microbiome. Regular physical activity and adequate hydration are also imperative for maintaining optimal gut function and overall health. Moreover, reducing stress through mindfulness practices, yoga, and adequate sleep can benefit gut health. Integrating prebiotics—non-digestible food ingredients that stimulate beneficial bacteria growth—into one’s diet can complement probiotic use, further promoting gut health and improving IBD outcomes. Foods rich in prebiotics include garlic, onions, asparagus, and bananas. Since gut health is multifaceted, adopting a holistic approach that encompasses diet, lifestyle modifications, and probiotics enhances the chances of achieving and sustaining remission. Understanding how various factors interact with the gut microbiome can empower patients to take control of their health journeys, utilizing probiotics as a valuable tool in the management of IBD.
Potential Risks and Considerations
Despite the benefits that probiotics may offer for individuals with Inflammatory Bowel Disease (IBD), certain risks and considerations warrant attention. Some patients may experience gastrointestinal discomfort, including bloating and gas when initiating probiotic therapy. It is advisable to start with lower doses and gradually increase to minimize adverse effects. Furthermore, individuals with compromised immune systems or those undergoing immunosuppressive therapy should approach probiotics cautiously, as there is potential for infections in such populations. Not all probiotics are created equal; the strain type, storage conditions, and expiration dates can impact the efficacy of the product. Therefore, it is vital to choose high-quality probiotics from reputable sources. Consulting a healthcare provider before beginning any probiotic regimen is essential, especially for individuals with complex medical histories or concurrent treatments. Ongoing research continues to explore the safety profile of probiotics in IBD, emphasizing the need for personalized evaluations. By being informed and proactive, patients can make educated decisions regarding probiotic use and maximize their potential benefits while minimizing risks.
The exploration of probiotics and their impact on Inflammatory Bowel Disease (IBD) is still evolving, with ongoing research providing new insights and evidence. Recent studies suggest that specific probiotic strains may possess anti-inflammatory properties, potentially playing a role in the modulation of immune responses within the intestines. Future research should focus on long-term studies to evaluate the safety and efficacy of probiotics in a broader population, intending to establish standardized guidelines for their use in IBD. Furthermore, understanding the mechanisms through which probiotics exert their effects could lead to the development of more tailored therapies for individuals showcasing varying symptoms and responses to existing treatments. Probiotic interventions hold promise in providing additional support for managing IBD, but they should not replace conventional treatments entirely. A collaborative approach combining traditional and complementary therapies can lead to improved health outcomes. By remaining engaged in research developments, healthcare providers and patients alike can maximize the potential of probiotics in enhancing the quality of life and well-being of those affected by this challenging chronic condition. As knowledge deepens, the therapeutic landscape for IBD may significantly improve.
In conclusion, probiotics offer valuable support in the management of Inflammatory Bowel Disease (IBD), promoting gut health and potentially alleviating symptoms. As research continues to advance, the understanding of how specific probiotic strains interact with the gut microbiome is set to evolve significantly. Probiotics may help restore microbial balance, enhance the gut barrier, and modulate immune responses, all essential for individuals battling IBD. However, due to individual variability in response and the complexity of gut health, it is essential to pursue a personalized approach. Individuals should incorporate a balanced diet rich in prebiotic and probiotic sources, alongside lifestyle modifications, to bolster overall gut health. The potential risks associated with probiotic use underscore the importance of discussing any intended probiotic regimen with healthcare professionals. As continuous studies shed light on the diverse roles of probiotics in gut health, patients can stay informed and empowered to make decisions that align with their health needs. Overall, the integration of probiotics into comprehensive treatment strategies represents a hopeful avenue for enhancing the health and well-being of individuals living with IBD.