The Impact of Chronic Illness on Depression and Treatment Strategies
Chronic illnesses can significantly affect mental health, especially concerning depression. People suffering from conditions like diabetes, cancer, or heart disease often have elevated levels of depression, impacting their quality of life. The chronic nature of these illnesses can lead to feelings of helplessness and hopelessness, exacerbating depressive symptoms. It is essential to understand how chronic illness intertwines with mental health to design effective treatment strategies. Mental health professionals must consider patients’ physical conditions when prescribing treatments, as the interplay between physical and mental health can complicate recovery. Numerous studies show that patients with chronic illnesses often display diminished response to traditional antidepressants. Therefore, managing chronic conditions alongside treating depression requires a multidisciplinary approach. Integrating medical care with psychological support can yield better outcomes. Holistic treatment plans encompass medications, therapy, as well as lifestyle changes, which can provide a more comprehensive support system for individuals suffering from both chronic illness and depression. Therefore, recognizing the connection between these issues is critical in creating effective treatment strategies that offer hope and improve overall well-being.
One crucial aspect of managing depression within the context of chronic illness is the role of social support. Emotional support from family, friends, or support groups can have a positive influence on an individual’s mental health. These connections help individuals feel less isolated and provide a sense of belonging and understanding. Engaging in community activities can enhance mood, decrease feelings of loneliness, and offer opportunities for shared experiences. Support groups, specifically designed for those facing chronic illnesses, can be particularly beneficial. Such groups allow individuals to share their challenges, coping mechanisms, and resources, which can help mitigate feelings of despair. Additionally, education on the illness and its effects on mental health can empower individuals to better manage their conditions. Many patients report improved mental health outcomes when they have access to information about their illness and treatment options. By fostering supportive environments and facilitating access to resources, both depression and its debilitating effects on chronic illness can be addressed more effectively. Building a strong support network is essential in the fight against the intertwined challenges of chronic illness and depression.
Understanding Treatments: Therapies and Medications
A key component in treating depression in patients with chronic illnesses involves a combination of medications and psychological therapies. Antidepressant medications may be prescribed; however, they must be carefully chosen based on the individual’s medical history and current medications. Some antidepressants can interact negatively with other chronic illness treatments, necessitating a thorough examination of the patient’s medications. Psychotherapy, particularly Cognitive Behavioral Therapy (CBT), has proven effective in addressing the complex emotional landscape many chronically ill patients navigate. CBT focuses on altering negative thought patterns that contribute to feelings of depression. Another method involves mindfulness-based therapies that help individuals develop coping strategies and improve overall emotional regulation. Integrating these therapies with physical treatments for the chronic illness can enhance outcomes. Additionally, treatment should also emphasize lifestyle changes, including diet, exercise, and sleep, which can significantly improve mental health. This holistic approach cultivates resilience, allowing patients to manage their chronic conditions and depressive symptoms together more effectively, ultimately aiming to improve their overall quality of life and mental wellness.
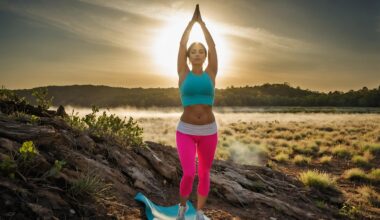
Regular physical activity has been shown to have profound effects on mental health, particularly for individuals dealing with both chronic illness and depression. Engaging in moderate exercise releases endorphins, which can elevate mood and reduce feelings of sadness. For chronic illness patients, tailored physical activity plans can also improve physical symptoms. Activities like walking, swimming, or yoga can increase energy levels, enhance flexibility, and promote relaxation. By incorporating exercise into treatment plans, healthcare providers can help patients combat both physical and mental health issues simultaneously. Additionally, the social aspect of group exercises can reduce feelings of isolation commonly experienced by individuals with chronic diseases. Even when physical limitations exist, adaptive exercises can ensure that patients remain active while respecting their health constraints. Establishing clear, achievable goals can foster a sense of accomplishment and motivation. Patients should consult with healthcare providers to develop personalized exercise programs based on their unique needs and limitations. Incorporating physical activity into daily routines can significantly impact patients’ mental health, ultimately helping them to maintain improved well-being throughout the treatment process.
Addressing the Stigma of Mental Health
Another important factor in managing depression among chronic illness patients is addressing the stigma surrounding mental health issues. Many individuals feel ashamed to admit they struggle with mental health, particularly when dealing with visible chronic conditions. This stigma can hinder individuals from seeking the help they need, perpetuating a cycle of isolation and despair. Education and awareness campaigns at community and institutional levels can help reduce stigma, making it easier for individuals to discuss their mental health concerns. Encouraging open conversations about mental health both in families and in healthcare environments can create supportive atmospheres. When seeking treatment, it is crucial that medical professionals approach the issue compassionately and without judgment to foster a sense of safety. Additionally, sharing stories of those who have successfully navigated the overlap of chronic illness and depression can provide hope and encouragement for others experiencing similar struggles. By dismantling the stigma surrounding mental health, more individuals may feel empowered to pursue help, resulting in better overall outcomes in managing their chronic illness and associated depression.
Ultimately, the intersection of chronic illness and depression has profound implications for patients’ overall health and recovery. It is vital to acknowledge that mental health is as critical as physical health when dealing with chronic conditions. Comprehensive treatment plans must integrate both medical care for chronic illnesses and focused mental health support. Collaborative care between healthcare providers, mental health specialists, and patients can produce the most effective results. This integrated approach allows for tailored therapies that address both depression and practical management of chronic illness. Furthermore, education about the mental health aspects of chronic illness for both patients and providers can improve understanding and promote more proactive approaches to mental well-being. Patients must feel empowered to advocate for their mental health needs alongside their physical health concerns. Recovery from depression and the management of chronic illness are achievable goals, particularly when approached thoughtfully and holistically. By employing a multifaceted strategy, individuals can work towards alleviating both their chronic illness and associated depression, ultimately enhancing their quality of life.
Conclusion: Combining Efforts for Healthier Lives
In conclusion, addressing the depression stemming from chronic illness requires a concerted effort from patients, healthcare providers, and the community. By acknowledging the complex relationship between chronic conditions and mental health, we can improve the well-being of those affected. It is imperative to prioritize awareness initiatives that educate both patients and providers about the interrelated nature of these issues. Continuous research into effective treatment strategies, including medications, therapies, and lifestyle modifications, must be emphasized to develop new approaches. Support systems play a vital role, providing emotional and practical assistance that fosters resilience and reduces isolation. Creating a supportive environment benefits not only individuals battling chronic illness but their families and communities as well. Ultimately, a comprehensive, integrated approach that combines physical and mental health care can enhance the quality of life for many individuals living with chronic illnesses. By treating both the mind and body, we ensure a more holistic healing process, allowing individuals to thrive, regain control of their lives, and foster a hopeful outlook on their health journey.
Furthermore, the collaboration between various healthcare professionals is essential in providing a comprehensive care plan. Multidisciplinary teams should work together to assess and address the unique needs of each patient, guiding them toward effective treatment options that cater to both their mental and physical health. This collaboration could involve primary care physicians, mental health specialists, nutritionists, and physical therapists, all working in tandem to create personalized strategies for each patient. Regular communication and shared goals among these professionals ensure a cohesive approach that tackles the intricacies of both chronic illness and depression. Thereby, fostering an environment where patients can thrive emotionally and physically. Encouraging patients to take an active part in their treatment plans and to voice their concerns can also improve adherence to prescribed therapies and overall satisfaction with their care. Engaging them in discussions about their specific needs and preferences fosters a sense of ownership over their health. Through this collaborative approach and active involvement, we can pave the way toward more effective treatment outcomes and improved quality of life for individuals facing the dual challenges of chronic illness and depression.