Genetic Insights Into Schizophrenia and Its Management
Understanding the interplay between genetics and schizophrenia offers significant insights into the disorder’s complexity. Schizophrenia is a severe mental health condition that affects how a person thinks, feels, and behaves. Genetic predispositions, alongside environmental factors, contribute to the risk of developing this disorder. Studies have identified numerous genes linked to schizophrenia, illuminating pathways that may influence neurotransmitter systems, neuron development, and cognitive processes. Identifying these genetic markers can aid in understanding individual differences in severity and response to treatment. For instance, individuals with certain genetic variants may exhibit a higher likelihood of treatment-resistant symptoms. This research also paves the way for personalized approaches to management, enabling targeted therapies based on genetic profiles. As a result, mental health professionals can devise more effective intervention strategies. Additionally, recognizing the genetic component can help in destigmatizing this complex condition. It allows families to understand that genetics plays a role, potentially reducing feelings of blame. Ultimately, genetic insights not only enhance our comprehension of schizophrenia but also emphasize the urgent need for continued research in mental health and genetics.
The Role of Genetic Studies in Understanding Schizophrenia
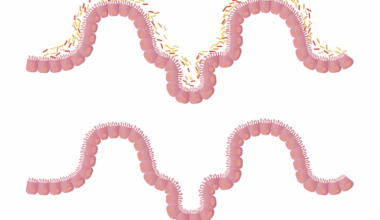
Genetic studies provide valuable information about schizophrenia’s heritability and underlying biological mechanisms. Twin and family studies have consistently shown that if one twin has schizophrenia, the other twin has a significantly higher risk of developing it. These observations point towards a strong genetic influence. Moreover, the advent of genome-wide association studies (GWAS) has revolutionized our understanding by identifying specific genetic variants associated with schizophrenia. These variants are often located in regions of the genome related to neuronal development and synaptic function. This genetic exploration leads to the identification of multiple biological pathways that may contribute to the disorder’s manifestation. For instance, alterations in dopamine signaling, a pathway significantly implicated in schizophrenia, can be traced back to certain genetic variations. By elucidating these connections, genetic studies help to refine diagnostic criteria and develop targeted interventions. Moreover, insights from genetic research underline the importance of integrating genetic counseling for affected individuals and families. Such measures can provide critical support, enabling individuals to navigate their condition more effectively. As research advances, the hope of employing genetics in clinical practice becomes increasingly attainable.
Another exciting development in the genetic understanding of schizophrenia is the exploration of epigenetics. Epigenetic mechanisms refer to modifications that affect gene expression without changing the underlying DNA sequence. Factors like stress, trauma, and substance misuse can lead to epigenetic changes that contribute to the onset and progression of schizophrenia. This perspective emphasizes that while genetics plays a crucial role, environmental interactions are equally significant. For example, individuals may carry genetic predispositions for schizophrenia, but environmental triggers may be necessary to activate these risks. Identifying these triggers is essential in both prevention and treatment strategies. Thus, a biopsychosocial approach to mental health management is vital. By combining insights from genetics, environmental factors, and psychological support, healthcare providers can develop comprehensive treatment plans. Furthermore, this approach aids in addressing stigma surrounding schizophrenia by providing a clearer picture of its multifactorial nature. The hope is to establish preventative measures that are rooted in both genetic and environmental awareness so that individuals can lead healthier lives. Moreover, understanding epigenetic influences might open doors to innovative therapeutic strategies in the management of schizophrenia.
Current Management Strategies and Genetic Considerations
Management strategies for schizophrenia traditionally involve antipsychotic medications, psychotherapy, and psychosocial interventions. These approaches focus on alleviating symptoms and improving overall quality of life. However, the variability in individual responses necessitates ongoing research into personalized treatment options. Genetic profiling may soon influence medication management, allowing healthcare providers to predict responses to specific antipsychotic medications. For instance, certain genetic markers can indicate a higher likelihood of adverse drug reactions, facilitating safer prescribing practices. Additionally, pharmacogenomic testing can help clinicians tailor dosages based on individual metabolic responses, improving efficacy and minimizing side effects. This growing field highlights the relevance of integrating genetic insights into clinical practice. Furthermore, coupling pharmacological treatment with therapeutic psychosocial interventions can offer additional support. Techniques like cognitive-behavioral therapy (CBT) and family therapy have shown effectiveness in managing symptoms. Education about the genetic factors of schizophrenia can empower patients and their families, fostering a supportive environment that encourages adherence to treatment plans. Ultimately, prioritizing personalized treatment approaches grounded in genetics will enhance outcomes and improve the overall management of schizophrenia.
A multi-faceted approach also considers the importance of lifestyle factors, including diet and exercise, in managing schizophrenia. Research suggests that lifestyle modifications can significantly impact overall well-being and symptom management. For example, certain diets rich in omega-3 fatty acids have been linked to improved mental health outcomes. Regular physical activity is also beneficial for reducing symptoms of anxiety and depression often associated with schizophrenia. Integrating lifestyle interventions with traditional treatment can create a holistic management plan. Mental health professionals should educate patients on the value of nutrition, exercise, and sleep hygiene in their overall management. Moreover, community support plays a critical role. Establishing supportive networks can aid individuals as they navigate their challenges. This approach fosters a sense of belonging and reduces isolation, which is crucial for mental health. Additionally, family involvement in the treatment process can bridge gaps in understanding, provide emotional support, and enhance treatment adherence. Attention to these factors can promote resilience and improve long-term outcomes. Considering lifestyle modifications in conjunction with genetic predispositions and therapeutic interventions could significantly revolutionize schizophrenia care in the future.
Future Directions in Genetic Research for Schizophrenia
The landscape of genetic research in schizophrenia is rapidly evolving, with new approaches continuously emerging. Advancements in technology, such as whole-genome sequencing, allow researchers to investigate the complexities of genetic contributions to the disorder more comprehensively. This technology can uncover rare genetic variants that may play a role in schizophrenia, broadening the scope of study beyond common variants identified in previous research. Understanding these rare variants may lead to new insights into disease mechanisms and potential therapeutic targets. Furthermore, integrating artificial intelligence in data analysis can expedite the identification of genetic patterns associated with schizophrenia. Machine learning algorithms can analyze vast amounts of genomic data to spot abnormalities that traditional methods might miss. As our understanding of the genetic determinants of schizophrenia deepens, the potential for novel treatment avenues emerges. Pharmacogenomic strategies may become standard in clinical practice, tailored to individuals’ unique genetic profiles. Additionally, research into gene-environment interactions will further illuminate the complexities of schizophrenia, paving the way for preventative strategies. Continued investment in research will ultimately enhance the effectiveness of management strategies and reduce the burden of this mental health condition on individuals and society.
In conclusion, understanding the genetics of schizophrenia is crucial for creating effective management strategies. Genetic insights offer vital knowledge that can refine how mental health professionals approach treatment. As noted earlier, insights from genetic studies can enable personalized treatments, improving medication efficacy and reducing side effects. Additionally, exploration of epigenetic factors reveals the importance of addressing environmental triggers for the condition. By cultivating supportive environments and prioritizing patient education, mental health systems can foster resilience among individuals with schizophrenia. Future research holds promise with advances in genetic technology and artificial intelligence. These developments will bolster our understanding of the disorder’s complexity. The fight against stigma surrounding schizophrenia is vital. By recognizing the genetic basis, society can promote compassion and understanding rather than blame. Leveraging genetic insights can help tailor strategies that align with individual needs, paving the way for comprehensive mental health care. Collaboration between researchers, clinicians, and patients will be essential in this evolving landscape. As we unravel the intricate web connecting genetics and schizophrenia, the hope is to improve outcomes for countless individuals affected by this challenging condition.
Ultimately, the future of schizophrenia treatment lies in integrating genetic research with innovative therapeutic strategies. The journey toward understanding this complex disorder is ongoing, but advancements are occurring rapidly. Collaborative efforts between geneticists, mental health professionals, and policymakers are critical in addressing the pressing issues surrounding schizophrenia. As genetic insights continue to inform treatment protocols, patients must remain at the center of these initiatives. By fostering a culture of empathy and support, communities can enhance the lives of those navigating the challenges of schizophrenia. As research progresses, it holds promise for identifying new targets for treatment, fostering resilience, and improving patient outcomes. Implementing genetic knowledge into everyday practice enhances therapeutic strategies, making care more personalized and effective. The ultimate goal is not just to manage symptoms but to deliver holistic care that considers the patient’s unique genetic landscape. Continued support for research and public awareness is key in minimizing stigma and promoting understanding. Embracing genetic insights is essential for revolutionizing how we approach schizophrenia treatment and care. By navigating this intricate landscape with hope and dedication, we can pave the way for a brighter future for individuals battling this mental health condition.