Understanding Allergies as an Immune System Disorder
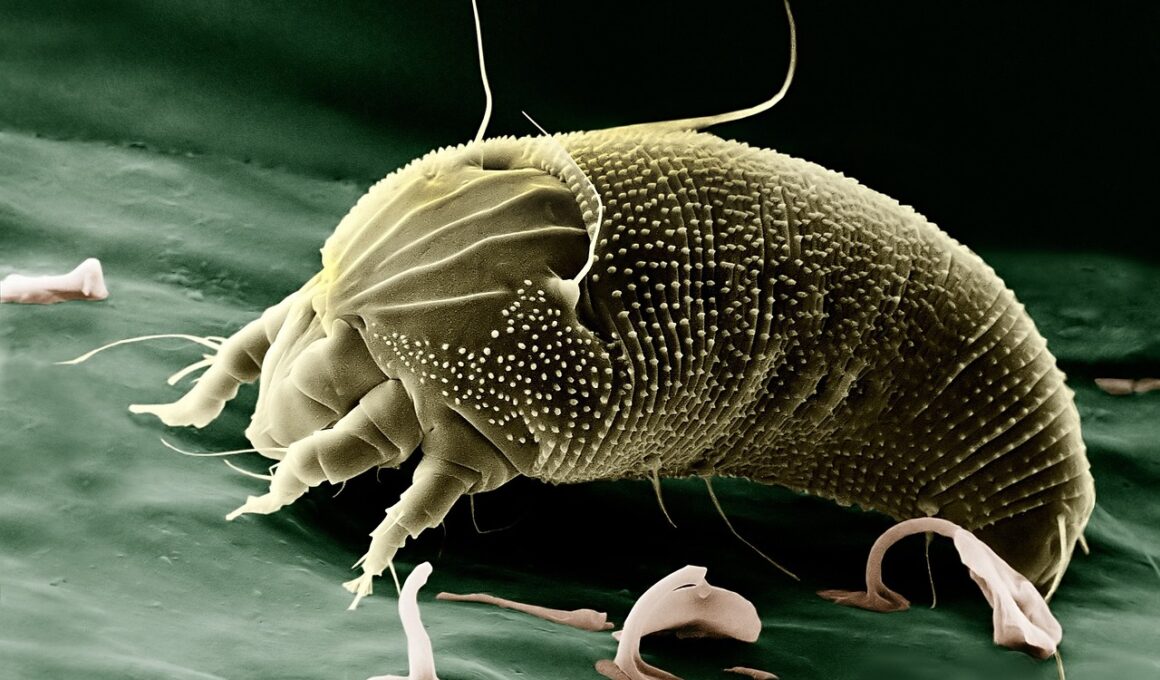
Allergies are common immune system disorders that occur when the body overreacts to typically harmless substances. These substances, termed allergens, can be found in various environments. Common allergens include pollen, dust mites, animal dander, certain foods, and insect stings. When the immune system identifies these allergens, it mistakenly deems them a threat, prompting an immune response. This reaction leads to an array of symptoms, such as sneezing, itching, rashes, and in severe cases, anaphylaxis. Anaphylaxis is a life-threatening condition that requires immediate medical attention. Allergies can manifest in different forms, such as hay fever, food allergies, and skin reactions like eczema or hives. Understanding the mechanisms behind allergies involves recognizing how genetic and environmental factors interact to trigger these immune responses. Furthermore, research indicates that exposure during early childhood may shape future allergic responses. Exploring allergies requires knowledge of the impact of lifestyle factors like diet and pollution on immune functions. Those affected can manage allergies through avoidance of known allergens and medications. Understanding allergies is vital for improving overall health and wellness, but it also can guide effective treatment strategies, enhancing the quality of life for sufferers.
Identifying specific allergens is crucial for managing allergies effectively. Allergists often conduct a variety of tests to determine what precisely triggers an individual’s allergies. Skin tests and blood tests are among the most common methods employed for this purpose. Through skin testing, a tiny amount of allergen is introduced into the skin, and reactions are observed. Alternatively, blood tests measure specific antibodies reacting to allergens. Once identified, avoidance strategies can significantly reduce symptoms. For food allergies, this may mean strict dietary restrictions. For environmental allergies, strategies can include using air purifiers and avoiding contact with pet dander. In some cases, immunotherapy may be recommended. This treatment gradually exposes the immune system to increasing amounts of the allergen, aiming to build tolerance over time. This process can take several months or years, but it offers long-lasting relief from allergy symptoms. However, immunotherapy is not suitable for everyone, and continued medical guidance is necessary for those considering this option. Education about allergies plays a pivotal role in prevention and management. Understanding different symptoms allows for timely responses, reducing the risks associated with severe allergic reactions.
The Role of Genetics in Allergies
Genetics significantly contribute to an individual’s susceptibility to allergies. Studies indicate that if one parent has allergies, the likelihood of their children developing them increases substantially. This hereditary pattern suggests that certain genes may influence the immune system’s responsiveness to allergens. Researchers have identified specific gene variations that relate to increased allergic reactions. These genetic factors likely interact with various environmental triggers, shaping individual responses. Lifestyle choices also intersect with genetics to create a complex web affecting allergies. Furthermore, environmental exposure during pregnancy and infancy may play a vital role in the development of allergies. For example, maternal diet during pregnancy can influence the child’s immune system. Similarly, early exposure to diverse foods and pets may lower the risk of developing allergies. Public health initiatives stress the importance of individualized approaches to allergy prevention based on a family’s specific history. Understanding these genetic factors and the environment’s role promotes better strategies in tackling allergies. Additional research continues to delve into how the microbiome, including gut bacteria, affects immune health and allergy development. Such insights are hopeful for future interventions and preventive measures.
Both allergic rhinitis, commonly known as hay fever, and allergic asthma illustrate the inflammatory nature of allergic reactions. Allergic rhinitis results when allergens in the air trigger symptoms primarily affecting the nose and eyes, leading to common complaints like sneezing, nasal congestion, and itchy eyes. Meanwhile, allergic asthma causes airway inflammation, manifested through symptoms such as wheezing, coughing, and difficulty breathing. The two conditions frequently co-occur, complicating the management of allergy sufferers. Environmental factors, including pollen count and air pollution, worsen symptoms. Consequently, residents in urban areas may experience higher rates of both conditions due to increased exposure to pollutants. Treatment methods play an essential role in alleviating symptoms. Antihistamines, corticosteroids, and bronchodilators are commonly prescribed medications. In addition, natural remedies like saline nasal rinses can offer relief. Ongoing research examines the efficacy of alternative treatments, such as immune-modulating therapies, showing promise for future treatment options. Managing quality of life for individuals with allergies involves proactive measures. Patients are encouraged to monitor symptoms, adhere to treatment plans, and maintain open communication with healthcare providers to adjust management strategies as necessary over time.
Understanding Anaphylactic Reactions
Anaphylaxis is an extreme and often life-threatening allergic reaction requiring immediate medical assistance. It differs from other allergic responses due to its intensity, often occurring within minutes of exposure to a trigger. Common anaphylaxis triggers include certain foods—such as peanuts, tree nuts, shellfish—and insect stings or medications. Symptoms range from hives and swelling to more severe complications like difficulty breathing and gastrointestinal distress. Recognizing symptoms early on is critical for effective intervention, as delayed treatment can result in severe complications. Epinephrine auto-injectors, often prescribed for those with known severe allergies, should be carried at all times. Knowledge of how to administer this medication is essential for anyone at risk for anaphylaxis. Patients and their families need to have an emergency action plan in place, ensuring that everyone knows how to respond effectively. Awareness about the condition encourages individuals to seek prompt medical care. Education plays a vital role in reducing anxiety for those facing anaphylaxis, equipping them with tools to navigate potential threats. Ongoing research into anaphylaxis continues to develop better understanding, aiming for effective preventative strategies and treatments to mitigate this severe reaction.
Food allergies exemplify one of the most common immune system disorders, particularly in children. They may present through mild to severe reactions, significantly affecting day-to-day life. Educators and caregivers can play a vital role in fostering safe environments for children with food allergies. Awareness and knowledge strengthen safety measures against unintentional exposures. The prevalence of food allergies has increased in recent years, with varying reports indicating affected populations. Common food allergens include peanuts, tree nuts, milk, eggs, soy, wheat, fish, and shellfish. Labeling regulations enhance consumer safety, requiring clear identification of allergens in packaged foods. Nevertheless, cross-contact during food preparation remains a significant challenge. Individuals with food allergies must diligently evaluate ingredients and, when necessary, consult with manufacturers to ensure compliance with dietary restrictions. Schools and childcare centers can promote safety through proper meal planning and communication with parents. Further research into food allergies aims to explore potential treatments. Desensitization methods, such as oral immunotherapy, are under scrutiny for their effectiveness. Understanding the complexities of food allergies fosters a more inclusive community, promoting informed choices and empowering those affected. Continued education can reduce stigma surrounding food allergies while enhancing overall understanding of this immune system disorder.
Environmental Factors and Allergies
Environmental factors play a significant role in allergic reactions, influencing immune responses critically. Among these, pollen stands out as a leading trigger, especially during certain seasons. Grass, ragweed, and tree pollen vary in levels throughout the year, significantly impacting people with seasonal allergies. Additionally, dust mites, molds, and pet dander can be found indoors, contributing to perennial allergic rhinitis. Air pollution also exacerbates allergic conditions by irritating airways, making symptoms worse for asthmatics. Increased allergens in urban areas correlate with levels of industrial activity, traffic emissions, and overall urbanization. Studies suggest that heightened pollution affects the immune system’s response to allergens by reducing its effectiveness. Lifestyle changes, such as time spent outdoors and maintaining clean indoor environments, can help mitigate these risks. Regular cleaning routines to reduce dust and implement efficient ventilation systems may also enhance indoor air quality. Importantly, understanding how environmental factors influence allergies can guide preventive measures. Awareness of pollen forecasts and pollution levels allows allergy sufferers to plan outdoor activities strategically. By addressing these environmental elements, individuals can take proactive steps to lessen the impact of allergies, ultimately improving their quality of life and health outcomes.
In conclusion, allergies are complex immune system disorders intertwined with genetic and environmental factors. Effective management requires understanding triggers, treatment options, and the importance of communication with healthcare professionals. Personal experience with allergies can deeply affect daily life, necessitating medical guidance. Individuals should learn to recognize their specific allergies and develop appropriate strategies for avoidance, as these proactive measures can greatly reduce risks associated with allergic reactions. Education is paramount in equipping individuals and families with the knowledge they need to navigate these challenges. Resources such as support groups and online communities offer valuable advice and encouragement for those dealing with allergies. As research continues to unfold, new therapies and interventions hold promise for better management of allergy symptoms. Individuals must stay informed about developments in allergy treatment and prevention. Taking an active role in one’s health can empower those with allergies to pursue a fulfilling life. Moreover, combating misconceptions about allergies furthers understanding and fosters compassionate responses within communities. Cultivating awareness around allergies ultimately enhances overall public health, leading to healthier environments and informed individuals better equipped to manage their allergic conditions.