The Relationship Between Gut Microbiota and Autoimmune Diseases
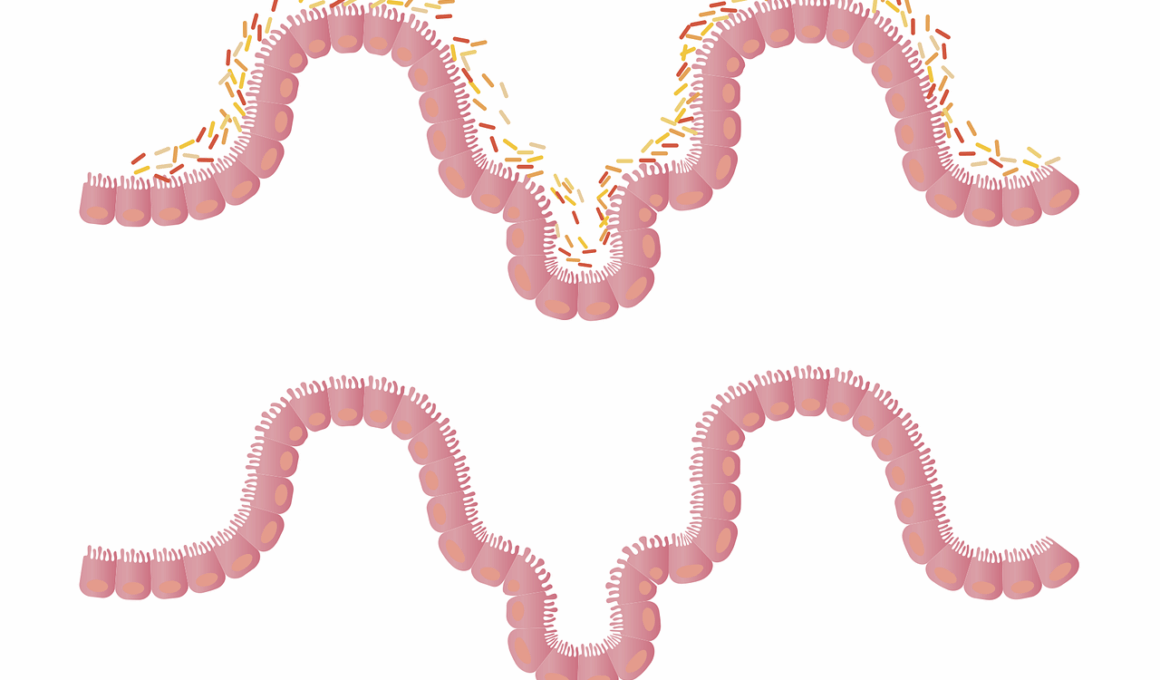
The gut microbiome plays a pivotal role in maintaining immune system health and balancing immune responses. The diversity of gut bacteria is essential for sustaining a healthy immune system. An imbalance, known as dysbiosis, may lead to altered immune functions, which can trigger autoimmune diseases. These conditions, characterized by the immune system attacking the body’s tissues, have been linked to changes in gut microbiota composition. Certain bacterial populations can contribute to inflammation, while others promote tolerance. This interplay showcases the delicate nature of our immune system and how gut health directly influences it. Additionally, emerging research suggests that diet significantly impacts gut microbiota composition and thus immune system efficiency. Consuming a diet rich in fiber and probiotics can support a healthy microbiome, potentially reducing the risk of autoimmune conditions. Moreover, understanding how specific gut bacteria interact with immune cells could open new avenues for therapy and prevention. Researchers are actively investigating dietary interventions and probiotics as potential treatments for those suffering from autoimmune disorders. Ultimately, our gut is far more than a digestive system; it is a key player in our overall immunity.
Several studies have drawn connections between specific gut bacteria and the onset of autoimmune diseases. For instance, patients with rheumatoid arthritis often display reduced diversity in their gut microbiome. Notably, certain bacteria, such as Faecalibacterium prausnitzii, are known for their anti-inflammatory properties and may offer protection against such diseases. In contrast, an abundance of Prevotella copri has been associated with heightened inflammation and disease severity in other autoimmune conditions. Furthermore, disruptions to gut permeability, often referred to as a ‘leaky gut,’ can exacerbate autoimmune responses. This allows unregulated passage of antigens and toxins into the bloodstream, further provoking immune reactions. Understanding these mechanisms is crucial for devising new treatment options. Since the gut microbiome interacts with both genetic and environmental factors, researchers are exploring potential therapies aimed at restoring healthy gut flora. From fecal transplants to tailored probiotics, microbiome modulation is an innovative approach that shows promise. As the links between gut health and autoimmune conditions become clearer, they present opportunities to develop novel prevention and management strategies for autoimmune diseases, aiming to enhance quality of life.
Diet and Its Impact on Gut Microbiota
Diet significantly shapes the gut microbiome and, by extension, the immune system. High-fiber diets promote the growth of beneficial bacteria that are crucial for maintaining gut health and immune function. On the contrary, diets high in processed foods can encourage the proliferation of harmful bacteria, contributing to dysbiosis. Research suggests that a Mediterranean-style diet, rich in fruits, vegetables, whole grains, and healthy fats, supports a diverse gut microbiome. Such a dietary approach could mitigate the risk of developing autoimmune diseases. Probiotics and fermented foods are also increasingly recognized for their role in supporting gut health. These foods introduce beneficial bacteria into the digestive system, enhancing microbial diversity. Prebiotics, found in foods like garlic and onions, serve as food for these beneficial bacteria, fostering a healthy environment. Additionally, individuals with autoimmune diseases may benefit from personalized nutrition plans that consider their specific gut microbiota profiles. Consequently, dietary interventions could prove effective in managing autoimmune health, potentially reducing symptoms and enhancing quality of life. Overall, diet is a powerful tool for optimizing gut health and supporting a robust immune response against autoimmune diseases.
In recent years, research has intensified regarding the role of the gut-brain axis in autoimmune diseases. This bidirectional communication between the gut and brain significantly influences immunological responses. Stress and mental health conditions can negatively impact gut health, leading to dysbiosis and immunological dysfunction. Chronic stress can alter gut permeability and microbiota composition, potentially triggering or exacerbating autoimmune diseases. Strategies that promote mental well-being, such as mindfulness and cognitive-behavioral therapy, may therefore indirectly benefit gut health. Additionally, addressing psychological stress could be crucial in managing autoimmune conditions holistically. Furthermore, neuroactive substances produced in the gut influences both mood and immune function, reinforcing the idea that emotional health is intertwined with gut health. Such findings emphasize the need for a multifaceted approach to treating autoimmune diseases, integrating psychological and nutritional aspects. Moreover, the microbiome’s influence extends to neuroinflammatory conditions, suggesting that interventions targeting gut health can have systemic benefits. As research evolves, the potential for harnessing the gut-brain axis in autoimmune healthcare presents exciting prospects, fostering greater awareness of the interconnectedness of mind, gut, and immune health.
Future Perspectives in Autoimmune Disease Treatment
The exploration of gut microbiota and its implications for autoimmune diseases holds significant therapeutic potential. Researchers are increasingly focused on understanding how microbiome manipulation can prevent or treat these conditions. Recent advances in genomics and metagenomics provide insights into individual gut microbiome profiles, paving the way for personalized medicine. Customizing treatment approaches based on unique microbiota characteristics may enhance efficacy and promote better outcomes. Administering live bacteria through probiotics is one promising avenue under investigation, with various strains showing potential for managing inflammation. Additionally, the idea of fecal microbiota transplantation is gaining traction, as it has shown promise in restoring microbial balance and improving health. The ongoing development of microbiome-targeted therapies could revolutionize the management of autoimmune diseases. While much remains to be learned, foundational research demonstrates that the gut microbiome’s influence on immune function is profound. This evolving field emphasizes proactivity in gut health as a proactive strategy for preventing autoimmune diseases. Much work is required to translate findings into widely applicable treatments. However, an emphasis on understanding the microbiome could significantly reshape healthcare practices surrounding autoimmune conditions in the future.
In conclusion, the relationship between gut microbiota and autoimmune diseases underscores the complexity of the human immune system. Maintaining gut health is vital for preventing and managing autoimmune conditions effectively. Dysbiosis appears connected to many autoimmune disorders, indicating the importance of a diverse and balanced microbiome. As research continues to highlight the role of diet, stress, and environmental factors in shaping our gut health, a comprehensive understanding emerges. The future of autoimmune disease management looks promising, particularly as we move towards microbiome-based therapies. By focusing on personalized interventions that incorporate dietary changes, probiotics, and addressing mental wellbeing, healthcare providers can develop patient-centered care strategies. As the science evolves, so too will our approaches to supporting a healthy immune system through gut health. Ultimately, integrating microbiome concepts into mainstream healthcare could lead to significant advancements in the prevention and treatment of autoimmune diseases. With growing awareness, there is potential for lifestyle modifications to become mainstream practices, leading to improved health outcomes for many individuals facing these challenging conditions. Staying informed about ongoing research and innovations is essential as we navigate this exciting intersection of gut microbiota and autoimmune disease management.
Final Thoughts
The implications of the relationship between the gut microbiome and autoimmune diseases extend beyond individual health. As communities become more educated about gut health, there is potential for a shift towards preventive measures at the public health level. Initiatives promoting healthy diets enriched with probiotics and prebiotics could reduce the incidence of autoimmune diseases over time. This may involve educational programs focusing on nutrition and gut health within healthcare settings. Additionally, future policies may prioritize research funding dedicated to unraveling the complexities of microbiota in relation to autoimmune disorders. Increased public awareness about the importance of gut health could empower individuals to take proactive steps in their lives. Ultimately, fostering a culture that values gut health and supports research initiatives can contribute to better overall wellness. With more resources allocated to exploring these connections, we may pave the way for innovative solutions to combat autoimmune diseases. As emerging findings and studies shape our understanding of this relationship, collaboration between researchers, healthcare providers, and communities will be crucial. By working together, the hope is to create comprehensive strategies aimed at promoting gut health to reduce autoimmune diseases in future generations.
The relationship between gut microbiota and autoimmune diseases is increasingly recognized in modern science. Emerging research shows a profound connection between gut health and autoimmune conditions, impacting immune system functions. The gut microbiome, made up of trillions of bacteria, influences inflammation, immunity, and even the likelihood of autoimmune disorders. An imbalance in gut bacteria, known as dysbiosis, can lead to inappropriate immune responses, triggering autoimmune diseases. This evidence emphasizes the importance of a healthy gut in preventing immune dysregulation. Maintaining a diverse array of gut flora is crucial for optimal immunity, with certain strains exhibiting protective properties against autoimmune conditions. As scientists continue to investigate the gut’s role in immune health, diet emerges as a critical factor. Nutrient-rich diets can foster the growth of beneficial bacteria, thereby reinforcing immune responses and reducing autoimmune risks. With greater understanding comes the potential for innovative dietary recommendations and treatments centered around gut health. Personalized nutrition aimed at bolstering gut microbiota may transform how autoimmune diseases are approached. Heightened awareness in both clinical and public domains underscores the urgency of maintaining gut health as a fundamental aspect of overall immune system support.