The Journey to a Successful Heart Transplant
Heart transplants represent a critical option for patients suffering from end-stage heart disease. The demand for heart transplants often surpasses the number of available organs, making the journey much more challenging for those in need. Preparing for a heart transplant involves rigorous assessments and tests, ensuring candidates meet specific medical criteria. This includes comprehensive evaluations of heart function, overall health, and psychological readiness. Potential recipients must understand the complexity of the procedure and possible complications. These assessments help determine eligibility for transplant lists. Continued medical advancements are helping to increase success rates and improve patient outcomes. Many centers provide educational resources to keep patients informed throughout the process. Understanding the need for lifestyle changes, including diet and exercise, is crucial in pre and post-transplant care. Support from healthcare professionals like nurses, dietitians, and mental health experts is essential. This holistic approach increases the chances of a successful transplant and promotes a better quality of life. Emotional preparedness and family support are also pivotal as they foster resilience throughout this arduous journey. With ongoing education and support, patients can become empowered participants in their care.
The waiting period for a suitable donor heart can be a daunting experience for patients. During this time, emotional and physical well-being may be at risk; therefore, psychological support plays a vital role. Many individuals experience anxiety or depression while waiting for a transplant; support groups can provide mutual encouragement. Strategies to manage stress include mindfulness, meditation, or engaging hobbies. Patients should stay proactive during the waiting period by adhering to medical advice, attending regular check-ups, and maintaining a healthy lifestyle. It is essential to stay connected with healthcare teams who can offer guidance on how to navigate this uncertain phase. Each day counts when waiting for an organ, and being well-prepared physically and emotionally can lead to better outcomes post-transplant. Additionally, making living arrangements, such as proximity to the transplant center, is crucial should an organ become available. Advancements in technology, including heart monitoring apps, can assist patients in tracking their health status. Those awaiting transplants should also consider involving family members in care plans, creating a better support system overall. Family involvement can help ease the burden of waiting and foster a sense of community and hope during this challenging time.
The Transplant Procedure Explained
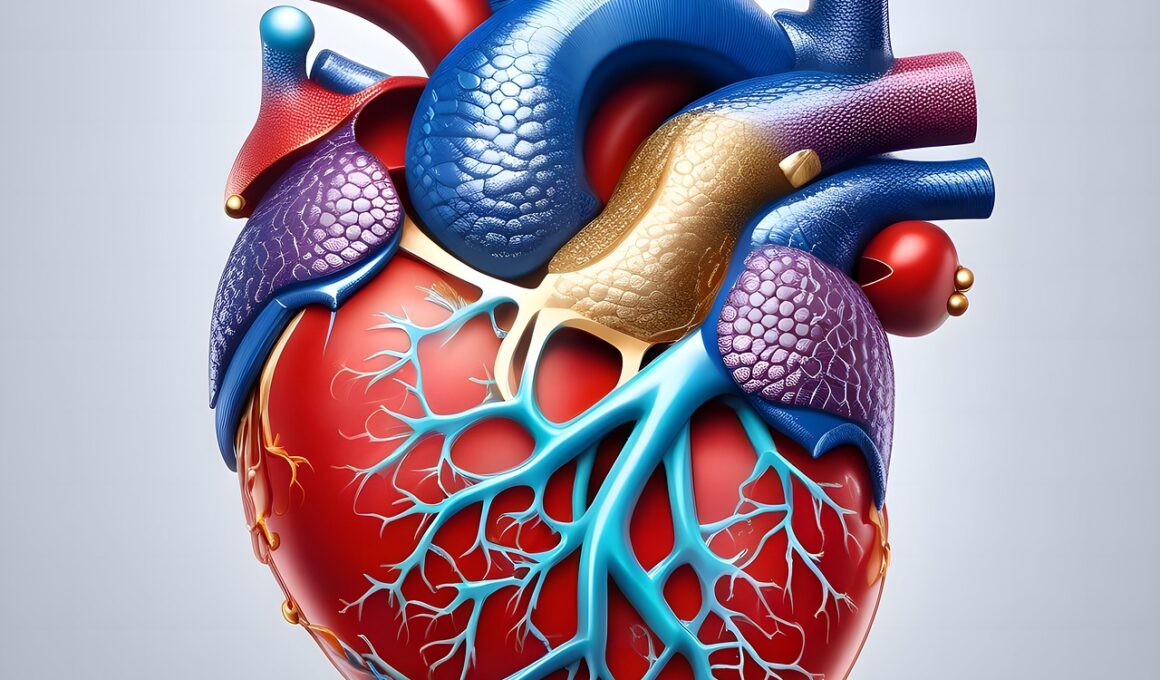
Once a suitable donor heart becomes available, the procedure begins with the patient being transported to the hospital. Anesthesia is administered, and the surgical team prepares the patient for the operation. The details of a heart transplant involve the careful removal of the damaged heart and its replacement with the donor organ. A skilled surgeon will make an incision in the chest, typically through the sternum, allowing access to the heart. Once the patient’s heart is removed, veins and arteries are carefully connected to ensure proper blood flow through the new heart. Advanced medical techniques and equipment allow for a more efficient and safer surgical process. The heart, once closely monitored, will be tested for proper function before the surgery concludes. After the transplant, patients are moved to recovery where close monitoring begins to observe how the body accepts the new organ. Awareness of the risk of rejection is crucial, and the patient will need to adhere to a strict medication regimen. Immunosuppressive drugs are vital to prevent rejection of the donor heart and must be taken diligently. This phase is critical for ensuring the transplant is successful and that the body adjusts well.
Post-operative care is immensely important for heart transplant recipients. Hospital stays may vary, typically lasting one to two weeks, during which healthcare providers closely monitor recovery. Medications to prevent organ rejection must be taken consistently. In addition, patients need to undergo regular check-ups to evaluate heart function and overall health. During this time, they should also focus on nutrition and adequate hydration. A balanced diet rich in fruits, vegetables, and whole grains is recommended, as it supports recovery and enhances overall well-being. Physical rehabilitation also starts soon after discharge, introducing light exercise tailored to individual capabilities. This promotes cardiovascular health, as physical activity is crucial for a successful recovery. Patients may need to initially limit strenuous activities until they gain strength. Besides physical health, emotional well-being is equally important. Counseling or support groups can provide outlets for sharing experiences and managing any feelings of anxiety or depression that arise during recovery. The journey continues as patients adapt to their new heart. Reconnecting with loved ones helps in regaining a sense of normalcy. Overall, a proactive approach to recovery leads to the best possible quality of life post-transplant.
Long-term Care and Management
Long-term care following a heart transplant is essential for maintaining the health of the new organ and overall patient wellness. Engagement with a healthcare team specializing in transplant care is crucial. Patients must keep all scheduled follow-up appointments, ensuring consistent monitoring of their heart’s function. These visits often involve blood tests, echocardiograms, and other assessments to confirm that the heart is functioning well. Additionally, adhering to the medication regimen prescribed by the healthcare provider is critical to avoid complications. Patients should stay informed about potential side-effects of medications, as some may experience difficulty in managing their regimen. Regular communication with doctors can help address any concerns. Lifestyle adjustments may include regular exercise, maintaining a healthy weight, and choosing nutritious foods. Avoiding tobacco and excessive alcohol consumption is crucial for heart health. Maintaining mental well-being through stress management techniques is equally important. Engaging in social activities can help mitigate feelings of isolation that may occur post-surgery. Overall, the approach to long-term care must be multifaceted and individualized. Empowering patients with knowledge leads to healthier lifestyles, bolstering the chances for longevity with their new hearts.
Emotional and psychological well-being play a vital role not only in the surgical journey but also in long-term recovery after a heart transplant. Patients may experience a range of emotions such as relief, anxiety, or fear once the transplant is successful. It is essential to address these emotions and develop coping strategies throughout the healing process. Many transplant centers provide access to mental health professionals as part of their care team. Using therapeutic techniques can help patients process their experience and learn to adjust to new realities. The impact of a heart transplant extends to family members as well, creating a shared journey of adjustment and emotional healing. Open communication within families can foster support networks, improving emotional resilience for all involved. Participating in support groups enables patients and families to share experiences, providing insight into the transplant journey. Educational resources on coping techniques and emotional support strategies are invaluable. Building connections with others who have undergone similar experiences can reinforce a sense of community. Continued education, emotional support, and psychological care increase the likelihood of adapting successfully. Prioritizing mental health will empower patients and their families as they navigate life post-transplant.
The Future of Heart Transplants
The future of heart transplants looks promising with ongoing advancements in medical technology and research. New techniques are constantly emerging, which help improve both the success rates and quality of life for patients. Innovations in organ preservation extend the viability of donor hearts, increasing the potential donor pool. Research into artificial hearts and assist devices is also gaining traction, offering hope for those who may not qualify for traditional transplants. These developments could provide alternative solutions for patients while they await a donor organ. Additionally, advancements in regenerative medicine could enable the potential to repair damaged heart tissue, minimizing the need for transplants altogether in some cases. Genomic medicine also promises a direct approach in customizing patient care, optimizing treatment plans based on genetic makeup. Increased awareness of unconscious bias in donor selection is crucial, and efforts are underway to ensure equitable access to heart transplants for all patients. Insurance reforms are also being advocated for, allowing more patients to receive necessary care. Research continues to revolve around minimizing organ rejection through innovative scientific approaches. These developments highlight that the field of heart transplants is evolving to create new possibilities for patients needing advanced cardiac care.