Understanding Insulin Therapy: A Comprehensive Guide for Diabetes Management
Diabetes management requires a thorough understanding of various aspects, including insulin therapy, which plays a crucial role for individuals with Type 1 and some with Type 2 diabetes. Insulin is essential for regulating blood sugar levels and allows glucose to enter cells, where it is utilized for energy. This process is hindered in diabetic patients, leading to complications. Insulin therapy provides a solution by delivering required insulin either through injections or insulin pumps. Healthcare providers determine the insulin type and dosage based on individual requirements, considering factors like age, weight, activity level, and dietary habits. By carefully balancing insulin treatment with other lifestyle interventions, individuals can maintain optimal blood sugar control. This therapy is often combined with dietary management and exercise to ensure comprehensive diabetes care. Patients must work closely with healthcare professionals to develop personalized treatment plans that meet their unique needs and to monitor their response to insulin therapy effectively. This collaboration enables patients to make informed decisions about their health and maintain a high quality of life.
Types of Insulin: Understanding Options
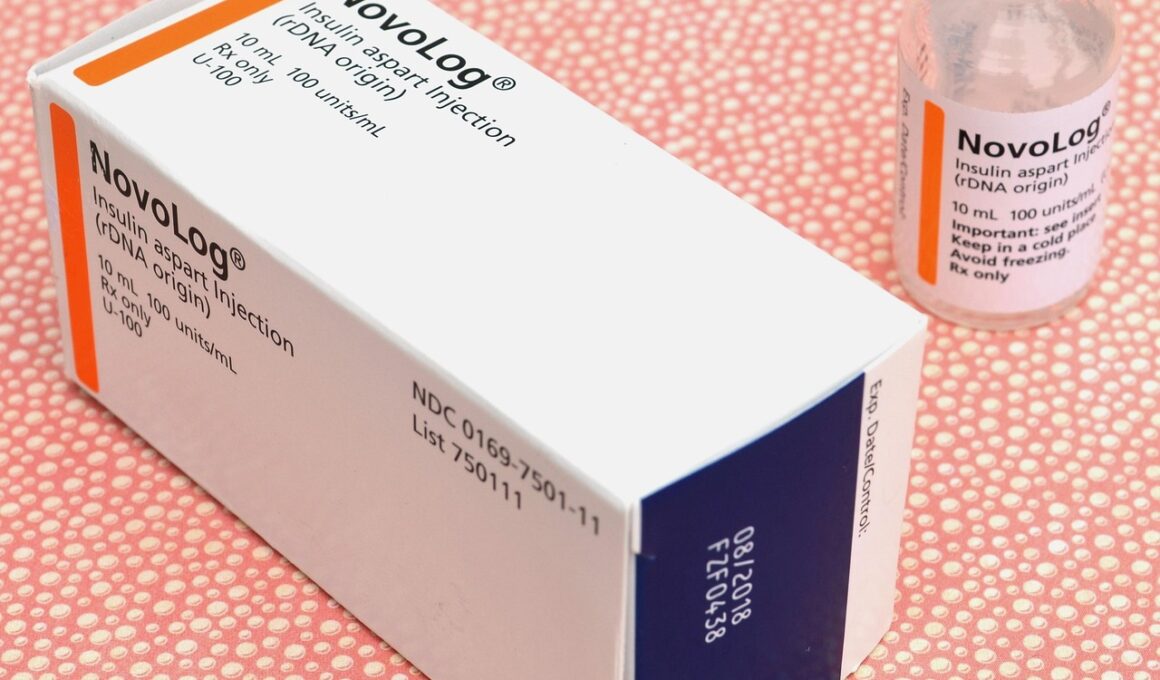
Various types of insulin are available for diabetes management, which each serves distinct purposes in controlling blood glucose levels. Broadly, the types are classified based on their onset, peak action times, and duration. Rapid-acting insulin begins to work within minutes but lasts for a short period, making it ideal for meal coverage. Short-acting insulin has a slightly longer duration and is often administered before meals. Intermediate-acting insulin provides a longer action profile, used to manage blood sugar levels throughout the day or night. Long-acting insulin offers a stable delivery of insulin over an extended period, reducing fluctuations in blood sugar. Some individuals may even utilize a combination of these types to suit their lifestyle needs effectively. Additionally, newer insulin formulations like insulin degludec provide flexibility due to their ultra-long action. Understanding each insulin type allows diabetics to make informed choices about their treatment. A proper regimen can lead to better health outcomes, improved quality of life, and greater freedom in daily activities, including meal planning and exercise.
Insulin therapy requires diligent monitoring of blood glucose levels to ensure proper adjustments in dosage. Regular glucose checks help patients understand their body’s response to insulin, allowing for timely intervention when levels rise or drop unexpectedly. Maintaining a detailed log of blood glucose readings can help identify patterns over time, which is essential for treatment adjustment. It is also vital for diabetics to recognize the signs of hypoglycemia and hyperglycemia. Hypoglycemia occurs when blood sugar becomes too low, leading to symptoms like dizziness, sweating, and confusion. On the other hand, hyperglycemia results from elevated blood sugar levels, which can cause excessive thirst, frequent urination, and fatigue. Both conditions require immediate attention and proactive management. Patients should work closely with their healthcare teams to adjust their insulin doses based on their readings and identify the necessity for additional intervention. Besides monitoring, education plays a critical role in ensuring that diabetics know how to effectively use insulin as part of their routine while mitigating any associated risks. Engaging in educational sessions can empower individuals to mastering diabetes management with confidence.
Administration Methods
Insulin delivery methods have evolved significantly, offering convenience and flexibility for users. One common method is via insulin syringes, which involves drawing up insulin and injecting it subcutaneously. While it remains widely utilized, some patients prefer the convenience offered by insulin pens. These pens come prefilled or can be loaded with insulin vials, providing a more discreet injection option. Additionally, insulin pumps are becoming increasingly popular, delivering a continuous supply of insulin through a small device worn on the body. Pumps allow users to customize their insulin delivery rates, making fine adjustments based on their activity level and meal intake. In recent years, advancements in technology have led to the development of continuous glucose monitors (CGMs), which track blood sugar levels in real time and can adjust insulin delivery automatically in some cases. These innovations not only improve convenience but enhance overall diabetes management by minimizing the risk of complications. Understanding these delivery methods and selecting one that best suits individual needs is crucial for effective diabetes management and achieving long-term health goals.
Beyond insulin, nutrition plays a pivotal role in diabetes management, influencing blood sugar levels and overall well-being. A balanced diet rich in whole foods, including vegetables, fruits, whole grains, lean proteins, and healthy fats, is beneficial for maintaining optimal health. Carbohydrate counting is especially important for those on insulin therapy, as it helps adjust insulin doses according to the amount of carbs consumed during a meal. Patients should focus on low glycemic index foods, which shed light on how foods impact blood sugar levels. Regular meals and healthy snacks spread throughout the day can help maintain steady glucose levels and prevent drastic fluctuations. Portion control should also accompany meal planning as excess calories can lead to weight gain, often complicating diabetes management. The role of a registered dietitian cannot be overstated; working with one can provide insights into meal planning tailored to individual preferences and lifestyles. Personalized dietary advice can empower patients to make healthier choices and foster independence in managing their condition while ensuring compliance with their insulin therapy regimen.
Exercise and Insulin Management
Physical activity is a crucial component in managing diabetes and can complement insulin therapy effectively. Regular exercise aids in enhancing insulin sensitivity, promoting better blood sugar control. It is essential for patients to engage in a variety of activities, including aerobic exercises such as walking, jogging, swimming, and strength training for overall fitness. Before commencing any physical activity, individuals should consult healthcare professionals to create a safe exercise plan tailored to their specific condition. Moreover, it is vital to monitor blood sugar levels before, during, and after exercise to prevent hypoglycemia. Some individuals may require a small snack before workouts to ensure they have adequate energy levels. Balancing exercise with insulin therapy may necessitate adjustments to insulin doses or carbohydrate intake, ensuring optimal blood glucose management. Establishing an exercise routine also offers psychological benefits, reducing stress and promoting a sense of well-being. Engaging in group activities or finding a workout partner can provide motivation and create a support system that encourages consistent engagement with healthy lifestyle choices.
Adapting to insulin therapy can be a significant transition for many individuals, requiring patience and perseverance. Feeling overwhelmed is common, as patients navigate their diagnosis, therapy, and changes to their daily routine. It is essential for them to understand that achieving balance in diabetes management is a journey that takes time and practice. Support networks, including family, friends, and diabetes support groups, can play a crucial role in providing encouragement and shared experiences. Mental health must also be addressed, as the stress of managing a chronic condition can lead to feelings of anxiety or depression. Seeking professional help when needed can be beneficial for many individuals. Furthermore, continuous education about diabetes and insulin therapy improves understanding and empowers patients to make informed decisions regarding their treatment. Participating in workshops, diabetes education classes, or online resources fosters a sense of community and shared learning. Ultimately, embracing the insulin therapy journey with an informed mindset and support can enhance motivation and inspire commitment to healthy living, promoting long-term success in diabetes management.
In conclusion, insulin therapy is a vital component of comprehensive diabetes management, requiring adaptability and continuous learning. By understanding the fundamentals of insulin types, administration methods, and dietary considerations, individuals can better navigate their treatment plans. Regular monitoring of blood glucose levels is essential for making informed decisions about insulin doses and lifestyle adjustments. Encouragement from healthcare professionals, along with a robust support system, can significantly impact adherence to therapy and promote a healthier quality of life. Engaging in regular physical activity enhances insulin sensitivity, enabling better blood sugar control when paired with insulin therapy. Recognizing that the road to successful diabetes management is a journey filled with ups and downs is crucial. Patience, education, and community support pave the way to resilience, empowering individuals to live fulfilling lives despite the challenges posed by diabetes. As technological advancements continue to evolve, patients have access to innovative tools that can aid in their management efforts. Staying informed about these advancements allows for more options in treatment and can foster optimism for better health outcomes. Ultimately, those committed to their health and armed with knowledge will find success in managing diabetes through insulin therapy.