Fasting and Its Impact on Gut Microbiome Composition
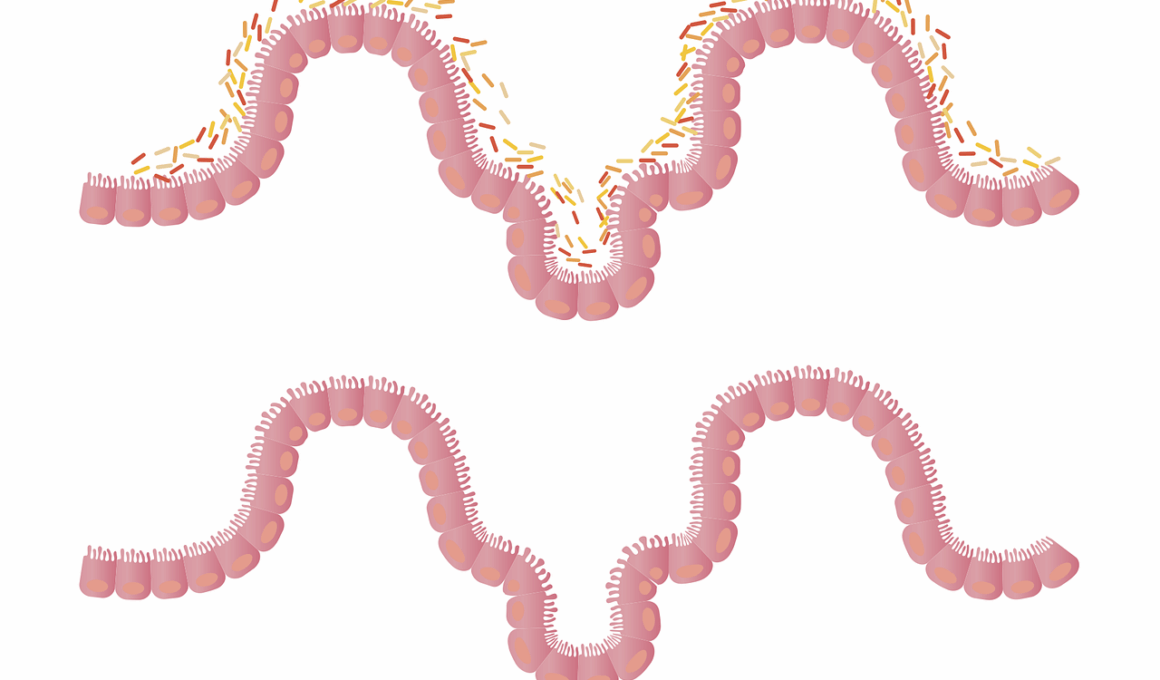
Fasting is a practice that has gained considerable attention in recent years, especially regarding its potential health benefits. One of the more fascinating areas of research focuses on the relationship between fasting and the gut microbiome. The gut microbiome comprises trillions of microorganisms that play a pivotal role in our overall health. Studies have shown that fasting can positively influence the composition of these microbial communities in the gut. This change can enhance gut health by promoting the growth of beneficial bacteria while reducing harmful strains. Consequently, individuals practicing fasting may experience improved digestion, a reduction in inflammatory markers, and better metabolic health. While eaters often consume food frequently, the break provided by fasting allows the gut to reset. As a result, the diversity of the microbial population can flourish during fasting periods. Various fasting methods, such as intermittent fasting, have shown promising results. Understanding the relationship between fasting and gut health opens new avenues for addressing metabolic disorders and improving overall health. This emerging area of research highlights essential insights into how lifestyle choices can profoundly impact gut microbiome composition and overall well-being.
The mechanisms underlying the impact of fasting on the gut microbiome are complex and still being investigated. Recent studies suggest that fasting can lead to the production of short-chain fatty acids (SCFAs), which are essential for gut health. SCFAs are produced when fiber is fermented by bacteria in the gut, and they play a significant role in maintaining the intestinal barrier. A strengthened barrier can prevent inflammation and promote a balanced immune response. Moreover, fasting can influence the metabolic pathways of gut bacteria, allowing them to thrive on different substrates during periods without food intake. This adaptability may enhance the resilience of the microbiome to shifts caused by diet or illness. Research indicates that fasting can also reduce the excess of certain bacteria associated with obesity and metabolic diseases. Instead, a more diverse gut microbiota composition can emerge, associated with better health outcomes. The process of fasting offers a reset, realigning our gut microbiome in beneficial ways. The focus on fasting is vital for developing innovative health strategies promoting our understanding of gut microbiome manipulation.
Fasting Methods and Their Microbiome Benefits
There are various fasting methods, including intermittent fasting (IF), alternate-day fasting (ADF), and time-restricted eating (TRE). Each of these approaches can uniquely influence gut microbiome composition. Intermittent fasting, for instance, is a popular method where individuals alternate between periods of eating and fasting. Research indicates that IF may lead to increases in beneficial microbial diversity. By allowing the gut to rest, beneficial bacteria can flourish, contributing to overall health. Similarly, alternate-day fasting allows for significant periods of fasting, which appear to provide gut microbiome benefits. Studies have shown that participants engaging in ADF exhibited favorable changes in gut bacteria associated with lower inflammation levels. Time-restricted eating, where eating is limited to specific hours of the day, also displayed positive effects on gut microbiome composition. This method supports the circadian rhythm of the gut, aligning eating patterns with the body’s natural rhythms, promoting optimal microbiome health. Thus, each fasting approach has unique advantages at the microbiome level, making understanding various methods crucial for those seeking gut health improvements.
Furthermore, the gut-brain axis becomes significantly relevant when considering the role of fasting in gut microbiome composition. The gut-brain axis refers to the complex communication between the gut and the brain, highlighting that the health of our gut microbiome can impact mental health. Evidence suggests that certain gut bacteria can produce neurotransmitters like serotonin, which plays a critical role in regulating mood. Engaging in fasting can alter gut microbiome composition, potentially leading to increased serotonin production, which may enhance mood and reduce anxiety. This relationship underscores the importance of nurturing the right bacterial balance. Moreover, fasting might also aid in reducing stress and inflammation, contributing to better mental health outcomes. As mental well-being continues to be a pressing concern, integrating fasting into one’s lifestyle may positively impact both gut health and mental health. Enhancing positive communication between the gut and brain may provide individuals with holistic health benefits. The growing body of research emphasizes the need for further exploration of fasting’s role in promoting psychological well-being through its effects on the gut microbiome.
Considerations and Precautions
While the potential benefits of fasting on gut microbiome composition are promising, it is essential to approach fasting cautiously. Individuals with specific health conditions or dietary restrictions should consult healthcare professionals before significantly changing their eating patterns. Those suffering from diabetes, eating disorders, or individuals with a compromised immune system could be at risk during fasting periods. Additionally, the quality of food consumed during eating periods significantly impacts microbiome health. Consuming a balanced diet rich in fiber, vitamins, and minerals is crucial to maximizing the benefits of fasting. Furthermore, hydration plays a vital role during fasting, as adequate water intake can further support digestive health. Making informed choices regarding what you eat during feeding windows determines the long-term effectiveness of fasting on gut health. It is essential to recognize that fasting may not be a suitable approach for everyone. Tailoring fasting methods according to individual circumstances is crucial for achieving optimal results. Therefore, careful consideration and professional guidance are advisable to safely engage in fasting and ensure that the benefits are maximized.
In addressing the intricate dynamics between fasting and the gut microbiome, dietary diversity plays an essential role. A varied diet provides the necessary nutrients that support a healthy microbiome, complementing the benefits derived from fasting. Research indicates that eating a range of foods can foster the presence of different beneficial bacteria, enhancing gut health. Engaging in fasting protocols should not eliminate dietary diversity during eating periods; instead, it should encourage the inclusion of various food types. This approach helps ensure that the microbiome remains diverse and resilient. Incorporating fruits, vegetables, whole grains, and fermented foods during feeding times can boost the overall effectiveness of fasting on gut health. Furthermore, the timing of meals can be critical. During eating windows, ensuring balanced nutrition can prevent the risk of nutritional deficiencies. Therefore, fasting should be adopted alongside a well-rounded diet that emphasizes diversity and nutrient density. This holistic approach to health ensures that benefits manifest across different areas of well-being. Ultimately, combining fasting with mindful eating habits can create a synergistic effect on gut microbiome composition.
Future Research Directions
Despite the promising findings regarding fasting and gut microbiome composition, extensive research is still needed. Future studies could explore the long-term impacts of various fasting methods on gut health across diverse populations. Understanding specific microbiome changes and how they correlate with specific fasting protocols may provide valuable insights. Additionally, more research is needed to investigate the role of individualized fasting strategies based on genetics, lifestyle, and existing health conditions. Addressing these variables will enhance the effectiveness of fasting interventions. Moreover, more clinical trials could help determine the direct health outcomes associated with fasting and gut microbiome changes. Gathering extensive data on microbiome responses to different fasting methods can enrich the scientific understanding of these dynamics. Exploring the connection between fasting and metabolic diseases is another avenue worth investigating. Delving into how fasting influences insulin sensitivity and metabolic health outcomes could yield valuable insights, particularly for those battling obesity or diabetes. Ultimately, a comprehensive understanding of fasting and its effects on the gut microbiome will facilitate the development of effective dietary interventions for better health.
In conclusion, the emerging relationship between fasting and gut microbiome composition offers exciting opportunities for enhancing health. Various fasting methods present unique benefits that contribute to a healthier gut environment. The impact on microbial diversity, SCFA production, and the gut-brain axis showcases the multifaceted nature of fasting in promoting better gut health. Nevertheless, it is crucial to approach fasting as a personalized journey tailored to individual health needs and circumstances. Ongoing research in this field will uncover more intricate connections that can guide individuals toward optimizing interventions for gut health. As we continue to explore this intriguing relationship, eliminating barriers to understanding the impacts of diet and fasting practices becomes increasingly important. By maximizing the benefits of fasting through informed choices, one can pave the way for improved physical and mental well-being. Engaging in fasting can lead us to cultivate healthier lifestyle choices, thus promoting longevity and overall happiness. As the body of knowledge grows, so does the opportunity for everyone seeking to unlock the profound benefits of fasting for gut microbiome health.