Influence of Environmental Factors on Gut Microbiome and Antibiotic Resistance
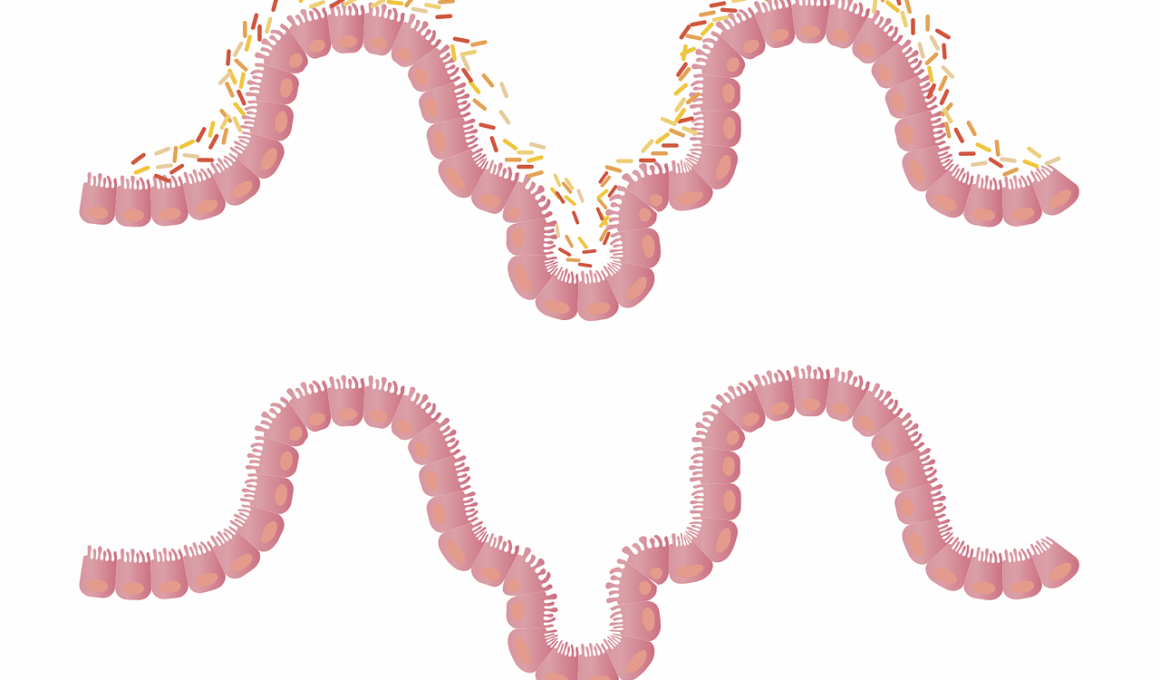
The gut microbiome plays a crucial role in the health of individuals, influencing immune responses and metabolic processes. This collection of microorganisms thrives in the gastrointestinal tract, adapting to the host’s conditions and environmental influences. Various factors, such as diet, lifestyle, and antibiotic use, can significantly affect the diversity and composition of gut microbiota. For instance, a high-fat and low-fiber diet often leads to a decrease in microbial diversity, which has been linked to conditions like obesity and metabolic disorders. Antibiotic usage, while essential for combating infections, can disrupt the balance of the microbiome, leading to an increase in antibiotic-resistant strains. These resistant microorganisms can pose serious health risks to individuals, as they limit treatment options for infections. The relationship between dietary habits and gut microbiome has been extensively studied, revealing that fermented foods rich in probiotics can enhance microbial diversity and resilience. Overall, maintaining a healthy gut microbiome is essential for overall health and protection against antibiotic resistance. Continued research is vital for understanding how to best protect and support our complex gut ecosystems.
In addition to diet, environmental exposure also plays a significant role in shaping the gut microbiome. Factors such as exposure to animals, soil, and certain pollutants can heavily influence microbiome composition. Studies have shown that populations with high exposure to rural environments tend to have a richer and more diverse gut microbiome. This diversity is often correlated with lower levels of allergies and autoimmune conditions. Conversely, urban environments, where there is a significant prevalence of sanitation and reduced exposure to various microbial sources, may lead to a less diverse microbiome. Furthermore, the usage of disinfectants and sanitation products can alter the microbial landscape both within households and on a broader scale within communities. Importantly, early exposure during childhood can set the stage for long-term immune health and microbiome stability. Research continues to explore the impact of various environmental factors on the microbiome, including how climate change may affect gut health indirectly through the food supply chain. Understanding these influences is essential not just for individual health but also for public health strategies aimed at combating antibiotic resistance.
The Role of Antibiotic Resistance in Gut Health
The rising concern surrounding antibiotic resistance has implications beyond clinical settings; it extends into public health and the ecosystem of the gut microbiome. Antibiotic treatment can decimate beneficial bacteria, leading to disturbances in gut flora. This disruption can create opportunities for the proliferation of pathogenic bacteria that may possess antibiotic resistance genes. As individuals experience recurrent infections, the cycle of antibiotic use continues, exacerbating the problem of resistance. The mechanism of resistance can vary, including the ability of bacteria to produce enzymes that deactivate antibiotics or modify their cellular targets. The presence of resistant gut bacteria highlights the urgent need to reconsider antibiotic prescribing practices. This includes promoting the use of narrow-spectrum antibiotics when possible, which are less likely to affect the entire microbiome. Probiotics and prebiotics have also gained attention for their potential to restore gut flora after antibiotic treatment. However, the efficacy of these interventions depends on various factors, such as timing and the specific strains used. In summary, the relationship between antibiotic resistance and gut health is complex and underscores the importance of a balanced microbiome.
Environmental pollution is an increasing concern that can also affect gut microbiome composition. The presence of heavy metals, pesticides, and industrial chemicals can alter microbial diversity and function. For example, exposure to heavy metals has been linked to shifts in microbiota that may lead to increased inflammation and the development of chronic diseases. This pollution problem needs addressing, especially in urban settings where industrial activity is more pronounced. Additionally, agricultural practices that utilize chemical fertilizers and pesticides can have downstream effects on the human gut microbiome through the food supply chain. Foods grown in heavily treated soils may harbor residues that impact human health when consumed. Increasing public awareness about organic farming methods and promoting access to organic produce can support healthier microbiomes. Moreover, reducing environmental pollutants through better waste management and emission controls can contribute to overall gut health. Studies demonstrate the significance of a clean environment in supporting diverse microbial populations. Therefore, tackling pollution is not just an ecological issue but also a health priority that reaches into our gastrointestinal health.
Dietary Patterns and Gut Microbiome Interactions
Dietary patterns significantly influence the gut microbiome’s composition, particularly through the intake of fiber, fats, and sugars. A diet high in refined sugars and low in dietary fiber has been shown to negatively affect gut bacterial diversity and richness. Consuming a variety of plant-based foods boosts the population of beneficial bacteria, which can aid in digestion and improve immune function. Whole grains, legumes, fruits, and vegetables are all sources of prebiotics, which support the growth of beneficial microbes. Fiber-rich diets promote the production of short-chain fatty acids, which are essential for gut health. The Mediterranean diet, characterized by high consumption of olive oil, fish, and fresh produce, has been associated with improved microbiome health and reduced inflammation. Furthermore, fermented foods such as yogurt, kimchi, and sauerkraut can introduce live beneficial bacteria to the gut. As we explore connections between dietary patterns and antibiotic resistance, of particular importance is how a healthy diet can minimize the risk of developing resistant strains. Overall, optimizing dietary intake is pivotal for supporting the microbiome and combating antibiotic resistance.
Emerging research continues to draw relationships between the gut microbiome, antibiotic resistance, and mental health. Gut microbiota interact with the central nervous system, influencing mood, behavior, and cognitive functions through the gut-brain axis. This bidirectional communication is pivotal for mental well-being, with research showing that dysbiosis—an imbalance caused by factors such as antibiotic overuse—can lead to increased risks of anxiety and depression. Prebiotic-rich diets not only benefit gut health but also appear to promote psychological resilience. Probiotics have also been studied for their ability to reduce symptoms associated with anxiety disorders. A balanced microbiome might support overall mental health, suggesting potential therapeutic approaches that target gut health for psychological benefits. The use of antibiotics, particularly during crucial developmental phases in young individuals, raises concerns about the long-term impacts on both gut microbiome and mental health. Strategies to minimize antibiotic usage and promote gut-friendly dietary practices could play a role in mitigating these risks. Understanding the links between gut health, mental well-being, and antibiotic resistance is vital toward achieving holistic health solutions.
Conclusion: Importance of a Balanced Gut Microbiome
Maintaining a healthy gut microbiome is essential for overall health and resistance to infections. Environmental factors, diet, and antibiotic use significantly impact the microbiome, promoting the development of antibiotic-resistant microorganisms. Awareness of these influences can guide individuals toward healthier choices for their gut microbiome, helping to prevent dysbiosis and related health issues. Actions to improve gut health may include increasing intake of fiber-rich foods, minimizing unnecessary antibiotic use, and reducing environmental pollutants. Probiotic and prebiotic supplementation also offers potential benefits. Future research should focus on understanding these connections more thoroughly, particularly how novel interventions could restore and maintain gut health. Communities must prioritize strategies that reduce pollution, promote organic practices, and educate individuals on dietary importance. For individuals, lifestyle changes that support the gut can lead to greater overall health benefits, enhancing quality of life. Ultimately, recognizing the integral role of the gut microbiome can lead to better health outcomes while addressing the challenges of antibiotic resistance. Through informed actions and community efforts, we can cultivate healthier microbiomes and promote lasting health.
It is essential to recognize the synergistic effects of various factors on gut microbiome and antibiotic resistance. With ongoing research, these insights pave the way for developing targeted interventions that can lead to improved health outcomes. Lessons learned from understanding the gut microbiome’s complexities can aid in curbing antibiotic resistance while enhancing our overall well-being. Society’s choices today can shape future public health, improving the state of our microbiota and with it, our health systems.