Understanding Caloric Needs during Pregnancy with Chronic Illness
Managing caloric intake during pregnancy can be challenging, particularly when a chronic illness is involved. Pregnant individuals must ensure that they get enough calories to support fetal growth while also managing their health conditions. Consulting with a healthcare provider or a registered dietitian can facilitate an individualized nutrition plan tailored to the specifics of the chronic illness. It is crucial to focus on calorie quality rather than just quantity, emphasizing nutrient-dense foods that provide essential vitamins and minerals. Foods rich in protein, healthy fats, and carbohydrates should be prioritized to provide the energy required during pregnancy. For those grappling with nausea or other pregnancy-related issues, it might be beneficial to consume more frequent small meals throughout the day. Additionally, hydration plays a vital role in supporting health and aiding digestion. Balancing caloric needs can further involve periodic assessments throughout the pregnancy to make necessary adjustments, ensuring both maternal and fetal well-being. Regular consultations with healthcare professionals and monitoring one’s symptoms may also guide dietary choices effectively, enabling an enjoyable pregnancy experience despite chronic conditions.
Understanding Energy Requirements
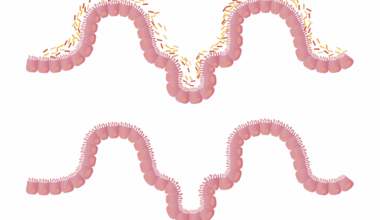
During pregnancy, energy requirements generally increase, but the extent varies based on individual health circumstances. Women with chronic illnesses may require personalized caloric assessments to establish their unique energy needs. This can be influenced by factors such as pre-pregnancy weight, the stage of pregnancy, and existing medical conditions. For instance, women managing diabetes may need to monitor their carbohydrate intake carefully, while those with thyroid issues might have fluctuating energy requirements. Understanding one’s basal metabolic rate (BMR) can help in determining the caloric needs during various pregnancy stages. It is important for the woman with chronic illness to engage in regular physical activity, as it not only aids in maintaining a healthy weight but also boosts overall energy levels. Balancing total caloric intake with activity levels can therefore help ensure sustained energy throughout pregnancy. Orchestrating a personalized approach by focusing on nutrient-dense meals can promote both fetal development and maternal health. To facilitate this, working closely with a healthcare provider will help design an optimal meal plan, adjusting calories according to feedback and emerging needs.
Protein intake becomes essential during pregnancy, especially for those with chronic illnesses. Protein helps in fetal growth and development, and it can also support maternal health. It is recommended to incorporate a variety of protein sources, including lean meats, legumes, dairy products, and plant-based options. In addition to sufficient protein intake, it’s important to focus on timing. Spreading protein consumption throughout the day can help stabilize energy levels and allow the body to absorb nutrients effectively. For individuals with chronic illnesses, tailored protein requirements may be needed based on different metabolic rates, making it crucial to consult a healthcare provider. Understanding how to efficiently combine proteins with other macronutrients, such as healthy fats and complex carbohydrates, is significant to enhance nutrient absorption. An example of a balanced approach includes pairing legumes with grains to increase the overall protein quality of a meal. Emphasizing flexibility in food choices can aid in accommodating taste preferences while ensuring adequate protein intake. Staying attentive to dietary preferences and restrictions becomes vital for maintaining a balanced diet that meets both caloric and nutritional needs.
Healthy Fats for Pregnancy and Chronic Illnesses
Healthy fats are critical for hormone production and cellular function during pregnancy. For expecting mothers coping with chronic illnesses, including sources of healthy fats in their diets can promote overall health. Focus on unsaturated fats found in avocados, nuts, seeds, and fatty fish. This can enhance nutrient absorption, which is particularly important for those with specific dietary restrictions. However, quality is key; trans fats found in processed foods should be avoided as they can exacerbate chronic conditions. Including sources of omega-3 fatty acids may benefit those with inflammatory conditions, promoting heart and brain health. While individuals with chronic illnesses should monitor their caloric intake, choosing the right kind of fats is essential. Portion control with fats helps in managing overall caloric intake while maintaining health benefits that come from these nutrients. Crafting a balanced diet that incorporates healthy fats should be done in consultation with healthcare professionals who can provide personalized recommendations. For those uncertain about specific food choices, resources from registered dietitians may assist in making informed, healthy eating decisions.
Carbohydrates provide necessary energy during pregnancy, but the focus should be on complex carbohydrates over simple sugars. This is particularly relevant for individuals with chronic illnesses who may experience blood sugar abnormalities. Whole grains, fruits, and vegetables offer sustained energy and prevent spikes in blood glucose levels. Establishing a diet with low glycemic index (GI) foods can be beneficial for maintaining balanced energy levels. A diet consistent with healthy carbohydrates may also assist in preventing excessive weight gain during pregnancy, which is crucial for those managing chronic conditions. Educating oneself on portion sizes and carbohydrate counting helps in keeping blood glucose levels stable. Pairing carbohydrates with proteins and healthy fats aids in maintaining fullness and satisfaction with meals. Given the individual needs during this period, pregnant women with chronic illnesses should work closely with healthcare providers to help design a diet that fits their health requirements. Versatility in food choices can ensure that individuals continue to meet their caloric needs without compromising on quality. Regular monitoring can further help in assessing caloric adequacy throughout the entire pregnancy.
Hydration and Its Importance
Hydration plays a pivotal role in ensuring healthy physiological processes during pregnancy, specifically when managing a chronic illness. Adequate fluid intake is crucial for digestion, circulation, and overall cellular function. Pregnant women should aim for increased water consumption to support amniotic fluid levels and provide hydration to tissues. For those with specific health conditions, it is crucial to monitor fluid retention and consult with healthcare providers for optimal intake recommendations. Remember that hydration can come from both liquids and water-rich foods, such as fruits and vegetables. Staying hydrated can boost energy levels and minimize common pregnancy discomforts, such as fatigue, headaches, and constipation. When living with a chronic illness, hydration status could influence symptom management and overall quality of life. Understanding personal hydration needs requires trial and feedback; thus, adjustments may need to be made during pregnancy to find an ideal routine. Personalized hydration strategies should be discussed with healthcare providers for satisfactory results. Monitoring urine color can also act as a simple indicator of hydration status and guide fluid intake throughout this vital period.
Planning meals that cater to pregnancy and chronic illness can enhance comfort and health outcomes. Utilizing meal planning can aid in managing caloric intake while streamlining grocery shopping. Creating a list of preferred foods that align with dietary restrictions and nutritional requirements is a beneficial approach. Preparing meals in advance allows for flexibility and variety while ensuring nutrient-dense choices are available at all times. A variety of foods can help in preventing meal fatigue, making it easier to stick to a healthy diet. Moreover, incorporating seasonal produce can enhance flavor and nutrition while reducing costs. Utilizing cooking methods that retain nutritional value, such as steaming or baking, can promote healthier meal preparations. Collaborating with a registered dietitian for meal planning assistance can also provide personalized insights tailored to unique health conditions. Families and partners can become involved in meal preparation to create a supportive environment that fosters healthy choices. Ultimately, maintaining an enjoyable meal experience is integral to adhering to dietary guidelines, ensuring success in achieving desired health outcomes throughout pregnancy while managing chronic illness.
Conclusion: Embracing a Nourishing Approach
Navigating the complexities of pregnancy with chronic illness necessitates a nurturing and adaptive approach to diet. It’s vital for an expecting mother to be aware of her body’s specific nutritional needs and to honor them. By prioritizing quality nutrition, such as healthy proteins, fats, and carbohydrates, the body can better cope with physical stresses and maintain optimal health. Regular communication with healthcare providers is key to achieving a well-rounded understanding of personal caloric needs as pregnancy progresses. By making informed decisions about diet and incorporating flexibility within meal planning, the journey can become more enjoyable. Building awareness and understanding of how chronic conditions affect nutritional needs creates a path for healthier choices. Support systems, such as family members or dietitians, can assist in making this journey more manageable. A nourishing approach to caloric needs promotes wellness for both mother and baby, fostering positive health outcomes during this pivotal life stage. Embracing this perspective significantly enhances the pregnancy experience, allowing for a positive experience despite the challenges posed by chronic illness. Thus, prioritizing self-care can enrich both maternal and fetal wellbeing.