The Influence of Chronic Stress on Gastric Acid Secretion
Chronic stress is known to significantly impact various bodily systems, and one critical area affected is gastrointestinal functioning. The interaction between chronic stress and stomach health is multifaceted, leading to notable changes in gastric acid secretion. This phenomenon can be understood through the perspective of the body’s stress response system, primarily the hypothalamic-pituitary-adrenal (HPA) axis. When faced with prolonged stress, the body produces elevated cortisol levels, which have been linked to various gastrointestinal disorders. Increased gastric acid secretion can lead to issues like gastroesophageal reflux disease (GERD) and peptic ulcers. The correlation between stress and digestive health has been the subject of numerous studies, emphasizing the need for a comprehensive understanding of this relationship. In particular, it is essential to consider factors such as diet, lifestyle, and psychological well-being in this context. Observing the effects of chronic stress on gastric acid can provide valuable insights into preventative measures and treatment options for individuals suffering from gastrointestinal ailments. Thus, recognizing chronic stress as a significant factor in gastric health is crucial for effective management and intervention.
Mechanisms Behind Stress-Induced Gastric Changes
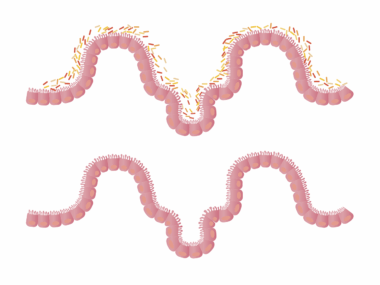
The mechanisms underlying the influence of chronic stress on gastric acid secretion are complex and multifactorial. One key factor to consider is the change in the autonomic nervous system’s regulation due to stress, which can enhance acid production. In stressful situations, the sympathetic nervous system increases the secretion of gastric acid, leading to an imbalance that may cause irritation. Moreover, stress can alter gastric motility, delaying the clearance of acid from the stomach. This alteration may expose the gastric mucosa to prolonged acid contact, increasing the risk of injury. Changes in gut microbiota composition are another potential mechanism through which stress influences gastric function. Stress may disrupt the balance of beneficial bacteria, leading to dysbiosis, which can further exacerbate digestive issues. Additionally, the psychological aspects of stress, such as anxiety and depression, can also influence perceptions of pain and discomfort, making it crucial to address mental health as part of treatment. Therefore, understanding how these mechanisms operate provides insight into strategies to mitigate the adverse effects of chronic stress on gastric acid secretion.
The effects of chronic stress on gastric acid secretion are also influenced by lifestyle factors, including diet and exercise habits. Nutritional choices play a critical role in gastrointestinal health, particularly during periods of stress. Diets high in processed foods, sugars, and unhealthy fats can contribute to worsening gastric disorders. On the other hand, incorporating whole foods, such as fruits, vegetables, and lean proteins, can enhance resilience against the negative impacts of stress. Regular physical activity is another essential component that helps mitigate stress effects and supports overall digestive health. Exercise promotes better stress management, improves mood, and enhances gut function. For many, mindfulness practices such as yoga and meditation can be effective in reducing stress levels. By adopting healthy lifestyle choices, individuals can bolster their gastrointestinal defenses against the detrimental effects of chronic stress. Addressing these factors collectively is crucial in managing gastric health and ensuring a balanced internal environment. As the understanding deepens about the interplay between stress, lifestyle, and gastric function, tailored interventions can be developed for those struggling with these interconnected issues.
Long-Term Implications of Stress on Digestive Health
The long-term implications of chronic stress on digestive health can be profound and multifaceted. Over time, chronic stress may lead to the development of severe gastrointestinal disorders, including inflammatory bowel disease and chronic gastritis. These conditions can significantly impair an individual’s quality of life and may necessitate ongoing medical intervention. Moreover, the psychological impact of living with chronic gastrointestinal disorders can further exacerbate stress levels, creating a vicious cycle that is difficult to break. Understanding the long-term consequences emphasizes the importance of early intervention and stress management strategies. Individuals experiencing chronic stress should work closely with healthcare providers to monitor gastric health proactively. This approach may involve regular screenings, lifestyle modifications, and nutritional counseling aimed at reducing the impact of stress on digestion. Importantly, holistic approaches that address both physical and mental health are vital for effective management. By recognizing the interconnectedness of stress and gastrointestinal health, effective preventative measures and treatment plans can be established, resulting in improved health outcomes for affected individuals.
In addition to lifestyle and psychological components, genetics can also play a role in how chronic stress influences gastric acid secretion. Genetic predispositions may affect an individual’s sensitivity to stress and their ability to cope with gastrointestinal disturbances. For example, certain genes linked to the regulation of the stress response may influence how efficiently the body produces gastric acid under stress. Research in this area is ongoing, and understanding genetic factors may help in tailoring interventions for those affected by chronic stress and gastrointestinal issues. Additionally, advancements in personalized medicine may provide opportunities for more effective management of stress-related gastric disorders. As the body of research expands, it is becoming increasingly clear that a multifactorial approach is necessary to address the myriad of factors influencing gastric health. Healthcare professionals must find ways to integrate these insights into practice, ensuring that patients receive comprehensive care that considers their unique genetic, psychological, and lifestyle factors. The goal is to develop targeted strategies that contribute positively to patients’ digestive health.
Practical Strategies for Managing Stress
Recognizing the significant impact of chronic stress on gastric health leads to the need for effective strategies to manage stress effectively. Aside from dietary changes and exercise, incorporating relaxation techniques into daily life can be highly beneficial. Techniques like deep breathing, progressive muscle relaxation, and guided imagery can help mitigate the body’s stress response. These practices encourage mindfulness, facilitating increased awareness of the body’s reactions to stress. Moreover, seeking support from friends, family, or mental health professionals can play an essential role in managing stress. Support groups or therapy sessions can provide valuable coping mechanisms and a sense of community. Engaging in hobbies or activities that bring joy can also serve as an effective outlet for stress relief. Ensuring adequate sleep is critical for maintaining overall health, as poor sleep can exacerbate stress and affect digestive function. Therefore, adopting a holistic approach to stress management, including physical, emotional, and psychological aspects, is paramount for fostering optimal gastric health and overall well-being.
In conclusion, the influence of chronic stress on gastric acid secretion is a crucial area of focus for both healthcare providers and individuals. The relationship between stress and gastrointestinal health underscores the importance of recognizing stress as a significant factor in digestive disorders. A comprehensive understanding of the mechanisms and lifestyle factors affecting this relationship can lead to more effective prevention and treatment strategies. As the field of microbiome research continues to expand, it will provide further insights into the connections between chronic stress and gastric function. Individualized approaches that encompass genetics, lifestyle, and mental health will likely yield the best outcomes for those affected. By prioritizing mental well-being along with physical health, effective interventions can be instituted to lessen the burden of chronic stress on gastric acid secretion. Ultimately, improving awareness and implementing actionable strategies can foster better health outcomes for individuals dealing with chronic stress and its impact on their gastrointestinal system. Adopting a proactive stance toward health is essential for promoting resilience and enhancing overall quality of life.
As a final note, further research in this field should aim to unravel the intricate relationship between chronic stress and gastric health. Interdisciplinary studies that combine psychology, gastroenterology, and nutritional sciences could illuminate new pathways for intervention. Future investigations should explore the role of psychobiotics, which may have the potential to influence gut health and alleviate stress-induced gastric disturbances as a novel treatment approach. Collaboration between researchers, clinicians, and patients will be key to understanding and improving care for those facing these challenges. Through continued inquiry and application of findings, it will be possible to establish best practices that promote healthy gastric acid secretion and overall digestive harmony. Addressing both the psychological and physiological aspects of chronic stress can pave the way for innovative therapies that enhance the lives of individuals living with stress-related gastrointestinal issues. By fostering a comprehensive understanding of the factors at play, healthcare providers can develop targeted interventions that improve long-term health outcomes and quality of life for affected individuals.