The Impact of Prenatal Nutrition on Future Mental Health and Suicide Risk
Prenatal nutrition plays a crucial role in shaping the mental health of offspring and their susceptibility to conditions like depression and anxiety in adulthood. Research indicates that a balanced diet rich in essential nutrients can positively influence brain development during fetal growth. Nutrients such as omega-3 fatty acids, folic acid, and vitamins B6 and B12 are particularly important. These elements contribute to neurotransmitter synthesis, which is vital for emotional regulation. When mothers consume adequate levels of these nutrients, it may reduce the risk of mental health issues later in life. Conversely, deficiencies in prenatal nutrition can lead to an increased risk of developing various psychiatric disorders. This highlights the importance of educating expectant mothers about nutritional choices. Interventions can be implemented in healthcare settings to support prenatal nutrition, ensuring that both mother and child have the best possible chance for a healthy life. This can directly relate to lower suicide rates, as mental health is a significant factor influencing suicidal thoughts and behaviors. As such, adequate prenatal nutrition should be a priority in public health programs.
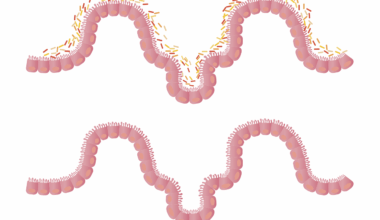
The association between prenatal nutrition and mental health outcomes extends further into early childhood stages. Children’s development is profoundly affected by their nutritional intake during pregnancy. Proper nutrients enable the development of neural pathways critical for cognitive and emotional health. Early exposure to rich nutrients helps in establishing a foundation for resilience against mental health issues. Studies have found that children born to mothers who ate a balanced diet have lower incidences of behavioral problems and depression. This indicates that prenatal dietary choices can carry long-term implications for mental stability. Additionally, the maternal gut microbiome appears to play a significant role, affecting not just health but also mental well-being. The maternal diet contributes to an optimal balance of gut bacteria, which can influence emotional outcomes for the child. Interventions such as dietary education and supplementation for pregnant women may yield substantial benefits for future generations. More research is needed to explore these intricacies and help develop targeted recommendations. By focusing on comprehensive prenatal care, we can enhance mental health outcomes and potentially reduce suicide rates later in life.
Nutrients Essential for Mental Health
Identifying key nutrients that promote mental health can guide maternal dietary choices. Omega-3 fatty acids, particularly found in fish and flaxseeds, possess anti-inflammatory properties and have been linked to improved mood regulation. Meanwhile, folic acid, found in leafy greens, is integral to brain function and can reduce the risk of postnatal depression. B vitamins play a critical role in the synthesis of neurotransmitters such as serotonin and dopamine, essential for emotional well-being. Pregnant women are often advised to incorporate these micronutrients into their diets to support brain development in the fetus. Iron and zinc are also vital, as they contribute to cognitive function. Deficiencies in these nutrients can lead to developmental delays and increased health concerns later on. Healthcare providers should emphasize the importance of a diverse and nutrient-rich diet during prenatal consultations. A holistic approach to prenatal nutrition, including supplementation when necessary, can foster healthier outcomes for children. Thus, it is essential that mothers be encouraged to prioritize their diets for the well-being of both themselves and their children.
Furthermore, the psychological impact of dietary choices cannot be underestimated. A mother’s emotional state greatly influences her eating habits during pregnancy. Stress and anxiety can lead to unhealthy eating behaviors, which may negatively affect fetal development. On the other hand, positive emotional well-being, often rooted in supportive community and family structures, encourages healthy eating habits. Prenatal counseling that addresses emotional and mental health needs can improve both maternal dietary choices and overall well-being. Cognitive Behavioral Therapy (CBT) techniques can also be implemented to help mothers cope with stress, leading to healthier dietary patterns. This spectrum of influence showcases the interconnectedness of mental health and nutritional intake during pregnancy. Healthcare systems need to provide adequate psychological support alongside nutritional guidance. By addressing mental health, pregnant women are better equipped to make informed dietary decisions. This creates a virtuous cycle, promoting both maternal and child health, potentially reducing long-term mental health issues. Therefore, integrating mental well-being with nutritional education should become commonplace within obstetrical care.
Long-term Mental Health Implications
The implications of prenatal nutrition on long-term mental health are profound. Children exposed to nutrient-rich environments in utero tend to exhibit better emotional regulation, cognitive functioning, and academic performance. This can be seen in studies showing reduced rates of attention-deficit/hyperactivity disorder (ADHD) and autism spectrum disorders in children whose mothers maintained a balanced diet during pregnancy. These outcomes underscore the relevance of maternal health on a child’s trajectory toward mental stability. Conversely, those born to nutritionally deficient environments may face chronic mental health challenges. Addressing prenatal nutrition not only helps individuals but can also reduce societal costs related to mental health care. By investing in prenatal nutrition initiatives, communities may witness a decline in healthcare expenditure linked to mental health disorders and related conditions. Additionally, the correlation between healthier nutritional practices during early development and lower instances of suicide later in life is compelling. This highlights the need for policymakers to prioritize public health campaigns focused on prenatal nutrition as a cost-effective strategy for improved mental health outcomes across populations.
Community engagement is vital for ensuring that future generations benefit from improved prenatal nutrition. Educational programs aimed at expecting families can facilitate awareness of the essential role nutrition plays in mental health. By partnering with healthcare providers, community organizations can effectively convey information regarding healthy eating during pregnancy. Workshops, nutritional classes, and cooking demonstrations can empower mothers to make informed dietary choices. Nutritionists can provide tailored guidance, ensuring that families understand not only what to eat but also how to incorporate these foods into their daily lives. Accessible resources such as e-books, mobile apps, and online platforms can further support this endeavor, bridging gaps in knowledge and access to information. Success stories from peers can be motivational, creating a shared culture surrounding positive health behaviors. Building social support networks among expectant mothers enhances the impact of these initiatives, fostering environments where healthy choices are prioritized. Ultimately, a community-based approach to nutrition education can empower families, setting a precedent for healthy lifestyles that contribute to better mental health outcomes and reduced suicide risks in the future.
Conclusion
In summary, the impact of prenatal nutrition is multidimensional and critical for future mental health. Nutritional choices made during pregnancy have far-reaching consequences for emotional well-being and cognitive development in children. By understanding the link between prenatal nutrition, mental health, and suicide risk, we can develop targeted interventions that support expectant mothers and their families. The integration of nutritional education and psychological support highlights the importance of a holistic approach in maternity care. By prioritizing these aspects, healthcare providers can strengthen the foundation of future generations while positively influencing mental health outcomes. Preventive measures taken during pregnancy can significantly affect a child’s lifelong journey, emphasizing the need for well-rounded prenatal care systems. Through educational outreach and community engagement, we can cultivate environments that promote better nutritional habits for expectant families. The resulting effects could lead to lower rates of mental health disorders and suicide risk, establishing a healthier society overall. Therefore, creating awareness and providing resources around prenatal nutrition must be a priority in public health policies moving forward.
The journey towards improved maternal and child health begins with recognizing the critical role of prenatal nutrition. As our understanding deepens, fostering a culture of health and well-being during pregnancy will create lasting changes in individual lives and entire communities. Research continues to uncover the nuances of how dietary practices influence mental health, paving the way for effective intervention strategies. Collaboration among healthcare providers, researchers, and community educators will be essential as we strive for holistic solutions. Advocating for accessible nutritional resources and support systems enhances the potential for successful outcomes in mental health for future generations. Finally, promoting these initiatives through policy reform will ensure that crucial knowledge reaches the families that need it most, further embedding mental health awareness into our cultural fabric. In conclusion, the impact of prenatal nutrition on mental health is an area worthy of exploration, investment, and prioritization for the betterment of all.