Genetics, Gut Microbiome, and Allergies: An Interconnected Story
The relationship between genetics, gut microbiome, and allergies is complex yet fascinating. Recent research indicates that our genetic makeup plays a significant role in determining not only our gut microbiota composition but also how our bodies respond to allergens. Individuals with a diverse and balanced gut microbiome are less likely to develop allergies. Factors such as diet, environment, and antibiotic use can influence this balance. An imbalance in the gut microbiome is linked with an increased susceptibility to allergic diseases. For instance, specific strains of bacteria, such as Lactobacillus and Bifidobacterium, have been shown to provide protective effects against the development of allergies. Furthermore, the immune system, which is closely tied to gut health, is influenced by both genetic predisposition and microbial diversity. Understanding this intricate relationship can lead to potential therapies targeting microbiome composition, thereby reducing allergic responses. Future studies must delve deeper into the specific mechanisms that connect these elements, paving the way for novel treatments that could alleviate allergy symptoms and even prevent their onset. Exploring genetic variants that impact gut health may further enhance our understanding.
The Role of Genetics in Gut Microbiome Composition
Genetic factors significantly contribute to the composition of the gut microbiome, influencing individual susceptibility to allergies. Various studies demonstrate that heritable traits can dictate the types of microbial communities present in the gut. For example, twins often share similar gut microbiota composition, providing evidence of genetic influence. Nonetheless, environmental factors, dietary choices, and lifestyle finalize this composition. Understanding the genetic determinants of microbiota can lead to personalized medicine approaches for combating allergies. Different genetic variants may affect an individual’s ability to metabolize certain foods or recover from gut disturbances. This variability can affect immune response pathways, directly linking gut health to allergy susceptibility. For instance, individuals carrying specific gene variants may also have a less diverse microbiome, which is often associated with increased allergy prevalence. Another element crucial to consider is epigenetics, where diet and lifestyle changes could alter gene expression without modifying the DNA sequence itself. Future research must focus on identifying specific genetic markers that contribute to variations in gut microbiota, which could eventually help in developing tailored interventions for individuals with allergic conditions.
The gut microbiome interacts intricately with the immune system, thereby influencing allergic responses. A well-balanced gut microbiome is crucial for educating the immune system and regulating its responses toward environmental allergens. Exposure to diverse microorganisms during early life promotes the maturation of the immune system, which critically reduces allergy risk. The hygiene hypothesis suggests that reduced microbial exposure due to modern living conditions may lead to an increase in allergic diseases. Consequently, individuals raised in rural versus urban settings often experience differing rates of allergies, attributed largely to microbiome diversity. Additionally, gut microbiome composition can modulate systemic inflammation, which is a key player in allergic reactions. Certain microbes can promote anti-inflammatory pathways, whereas others may exacerbate the inflammatory responses associated with allergies. This knowledge opens new doors for potential therapeutic strategies that target gut health to modulate the immune response. Probiotic supplementation and dietary interventions are gaining interest as means to alter the gut microbial landscape favorably. Focusing on the gut-brain axis could also provide insights into how gut health impacts anxiety and stress, factors known to exacerbate allergic reactions.
Allergic Diseases and Their Connection to Gut Health
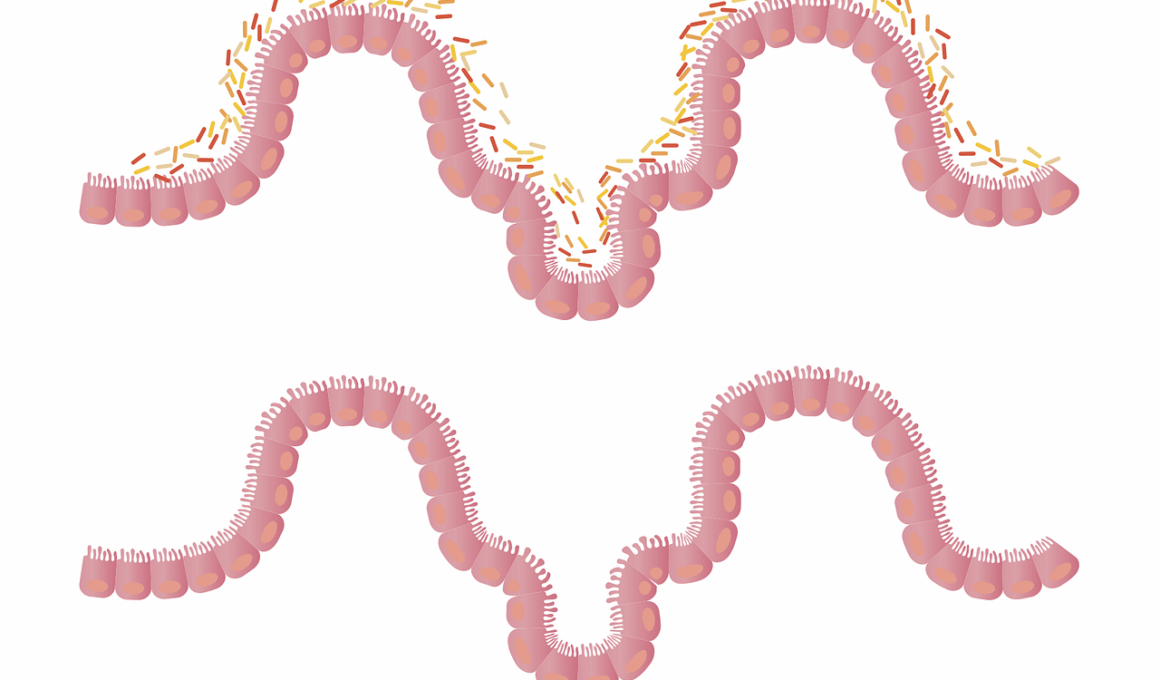
Allergic diseases, such as asthma, hay fever, and food allergies, are increasingly prevalent worldwide. Understanding the connection between these conditions and gut health is becoming an area of significant research. Recent findings suggest that an unhealthy gut microbiome can be a contributing factor to the onset of allergic conditions. Particularly, microbial dysbiosis, characterized by a lack of beneficial bacteria and an abundance of harmful species, can lead to an inappropriate immune response towards harmless environmental substances. For example, alterations in the gut microbiome can increase intestinal permeability, sometimes referred to as “leaky gut,” allowing larger antigens to enter the bloodstream and trigger allergic reactions. Certain diets lacking in fiber and high in processed foods may exacerbate dysbiosis, resulting in increased allergy risk. However, adopting a diet rich in fruits, vegetables, and fermented foods can foster a more diverse microbiome. This connection between dietary patterns, gut health, and allergic diseases highlights the potential for dietary interventions as effective means for allergy prevention and management. Addressing gut health through appropriate lifestyle modifications can lead to significant improvements in allergic disease outcomes.
Emerging evidence highlights the potential benefits of probiotics in managing allergies by modulating the gut microbiome. Probiotics are live bacteria that, when ingested in adequate amounts, confer health benefits to the host. Clinical studies have shown that specific probiotic strains can help reduce allergic symptoms, particularly in children. For instance, some research reports a reduction in the severity of eczema and respiratory allergies associated with early probiotic introduction. However, not all probiotics are equally effective, as strain-specific responses vary among individuals. Thus, personalizing probiotic therapy based on genetic and microbiome profiles may enhance efficacy. In addition to probiotics, prebiotics, which are dietary fibers that feed beneficial gut bacteria, can also play a significant role in improving gut health. Diets rich in prebiotics may support the growth of protective bacteria, thus increasing microbiome diversity and function. Co-administration of probiotics and prebiotics has garnered interest as a strategy to synergistically enhance gut health, potentially lowering allergy risk. More extensive and rigorous clinical trials are necessary to determine optimal strains and dosages for the suitable management of allergies through gut microbiome modulation.
Future Directions in Allergy and Gut Microbiome Research
As the research connecting gut microbiome and allergies continues to evolve, several future directions are emerging that warrant further investigation. One area of focus is the timing of microbial exposure during a child’s development, emphasizing early-life interventions to promote healthy gut flora. Understanding how the microbiome develops and its implications for immune tolerance is crucial. Another significant aspect is investigating the role of specific dietary patterns or nutrients that can support a healthy gut microbiome and, in turn, modulate allergic responses. For instance, the inclusion of fiber-rich foods, polyphenols, and omega-3 fatty acids may have favorable impacts on gut microbiota composition and immune function. Environmental factors, including exposure to pets and urban versus rural living, also need thorough exploration. Integrating modern genomic techniques such as metagenomics and metabolomics into studies will enhance understanding of complex interactions between microbiota and host genetic factors. Recognizing how these interactions drive allergies may lead to innovative preventive and therapeutic strategies. Future interdisciplinary collaborations within microbiome, genetic research, and allergology will be pivotal in shaping effective interventions for allergic diseases.
In summary, the intricate relationship between genetics, gut microbiome, and allergies offers exciting possibilities for enhancing health outcomes and allergy prevention. Individuals’ genetic predispositions shape their gut microbiota composition, which in turn influences immune responses to environmental allergens. This interconnected story urges the need for further research into key microbial species, genetic markers, and environmental factors that contribute to the development of allergies. Emphasizing personalized medicine approaches targeting gut health can lead to tailored interventions based on an individual’s genetic makeup. With the rise of probiotic and prebiotic treatments, there exists potential to leverage these strategies to safeguard against allergic diseases. Exploring dietary recommendations aimed at boosting microbial diversity is essential. Engaging in broader initiatives that promote healthy gut environments from early life may be key in combating soaring allergy prevalence rates worldwide. As ongoing studies uncover more about the gut microbiome’s role in health, the prospect of developing effective prevention and management strategies appears promising. The intertwined nature of these factors highlights how a multifaceted approach is essential for addressing allergic diseases.