Brain-Computer Interfaces and Their Role in Early Detection of Cognitive Disorders
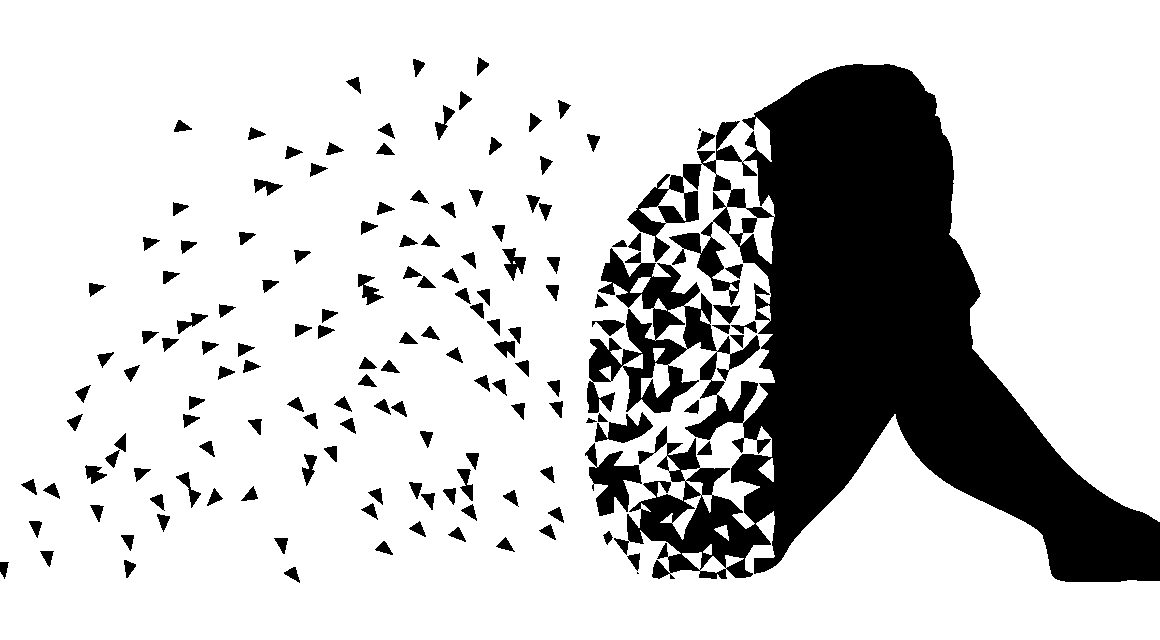
In recent years, there has been a significant advancement in the field of brain-computer interfaces (BCIs) and their potential to revolutionize cognitive health monitoring. These devices create a direct communication pathway between the brain and external systems. By interpreting neural signals, BCIs can provide insights into cognitive function and health. This capability opens new avenues for the early detection of cognitive disorders. The increasing prevalence of conditions such as Alzheimer’s and dementia underscores the importance of early intervention. BCIs allow for continual monitoring, enabling timely clinical responses. They harness neural activity data, ensuring that changes in brain function are detected even before behavioral symptoms manifest. Furthermore, researchers have developed algorithms to analyze complex brain activity patterns, identifying anomalies that may indicate the onset of cognitive issues. By pinpointing these changes early, individuals can benefit from preventive measures, enhancing their quality of life. This shift in paradigm showcases the immense potential of embracing technology in cognitive health, offering hope for millions affected by cognitive decline. As we continue exploring these technologies, ethical considerations regarding privacy and data security also emerge.
The technical aspects of how brain-computer interfaces operate are essential for understanding their significance in cognitive health. BCIs function by using electroencephalography (EEG) to capture brain activity, translating these signals into actionable data. The neural signals are recorded via sensors placed on the scalp, allowing for non-invasive monitoring of brain activity. By employing advanced machine learning techniques, algorithms process the vast amount of neural data obtained, identifying specific patterns that correlate with cognitive states. This computational analysis is crucial as it helps in recognizing deviations from an individual’s baseline brain function. For example, atypical brain wave patterns may signal cognitive impairment before observable symptoms arise. BCIs are not limited to diagnostics; they can also facilitate rehabilitation by providing real-time feedback to users, allowing them to practice cognitive tasks effectively. Therefore, BCIs represent a dual approach: assessing cognitive function and offering cognitive exercises. As technology progresses, the resolution and accuracy of neural data capture are expected to improve, making BCIs even more reliable for early detection. Therefore, incorporating BCIs into routine health assessments can lead to significant enhancements in cognitive health monitoring.
The Benefits of Early Detection of Cognitive Disorders
Detecting cognitive disorders early can transform treatment and management outcomes profoundly. Early intervention strategies can mitigate the progression of neurodegenerative diseases, resulting in better patient quality of life. Cognitive assessments that utilize brain-computer interfaces provide real-time feedback about brain health and potential risks. This proactive approach to cognitive health enables healthcare providers to customize care plans tailored to individual needs. By assessing cognitive function regularly, changes can be noted and addressed before they escalate into more severe conditions. Moreover, early detection allows for educational initiatives aimed at increasing awareness about cognitive decline. Patients and caregivers can benefit from understanding cognitive health, leading to prompt action. BCIs also serve to engage patients in their healthcare journey, fostering a positive outlook on managing their cognitive health. Furthermore, educational programs can help relatives of those at risk, emphasizing the importance of monitoring cognitive function and encouraging adaptable lifestyle choices. In doing so, BCIs encompass a holistic strategy toward cognitive health, integrating technology, education, and personal agency for better health outcomes.
Brain-computer interfaces also present exciting possibilities for personalized medicine in cognitive health. As BCIs gather extensive data on individuals’ brain activities, they facilitate a deeper understanding of individual cognitive profiles. This data-driven approach allows healthcare professionals to design interventions that suit each patient’s unique cognitive fingerprints, moving beyond the traditional one-size-fits-all solutions. Personalized cognitive rehabilitation programs can be developed through BCIs, capitalizing on specific brain activities associated with functions such as memory and attention. The potential for tailored cognitive exercises makes rehabilitation more effective and engaging for users. Furthermore, BCIs can help in monitoring the effectiveness of personalized interventions over time, allowing adjustments based on real-time feedback from brain activity. This adaptability is crucial as the condition of cognitive decline can vary significantly from one individual to another. With technology continuing to advance, we can expect even more sophisticated personalization, which may lead not only to capturing cognitive impairments effectively but also enhancing cognitive resilience. Engaging with brain-computer interfaces thus represents a promising avenue toward improved individualized patient care.
Challenges in the Field of Brain-Computer Interfaces
Despite the promising advancements, utilizing brain-computer interfaces for early detection poses several challenges. One of the primary hurdles is ensuring the reliability and accuracy of the data collected from neural activity. Variability in individual brain activity can sometimes lead to false positives or negatives, complicating diagnoses. As such, further research is necessary to refine algorithms that interpret EEG data effectively. Moreover, the user experience of BCIs is critical. For widespread acceptance, these interfaces must be easy to use and comfortable for individuals. Ensuring accessibility for diverse populations, including the elderly and those with disabilities, is vital to make these technologies beneficial for everyone. Additionally, ethical concerns surrounding data privacy and consent are paramount. Individuals must trust that their neural data will be handled with the utmost respect and security. To address these issues, regulatory frameworks must be established that govern the use of BCIs, ensuring users’ rights and privacy are upheld. As these challenges are met with innovative solutions, the potential for BCIs in cognitive health could flourish, leading to enhanced monitoring and intervention capabilities.
The future of brain-computer interfaces in the realm of cognitive health looks promising yet requires ongoing collaboration among various fields. Interdisciplinary partnerships involving neuroscientists, engineers, psychologists, and healthcare providers are essential to advancing the technology and its applications. Continuous improvement in BCI design, alongside educational initiatives for both clinicians and patients, can facilitate better deployment and acceptance of this technology. Furthermore, addressing the ethical and social implications of BCIs will ensure that advancements align with public interest and trust. As we look ahead, the potential for integrating BCIs with artificial intelligence is also an exciting frontier. This combination could facilitate even greater insights and predictions regarding cognitive health trajectories and interventions. Additionally, there is potential for enhancing community outreach, increasing awareness, and understanding of cognitive disorders and the role of BCIs in prevention and management. Engaging patients, families, and the healthcare community will create a supportive ecosystem where BCIs are embraced as essential tools for cognitive health monitoring. Therefore, the collective effort toward advancing BCIs will significantly impact early detection and intervention.
Conclusion
In conclusion, the integration of brain-computer interfaces in early detection of cognitive disorders represents a transformative opportunity within cognitive health. These devices not only monitor cognitive function but also pave the way for personalized interventions that can significantly enhance patient outcomes. Early detection through BCIs allows for timely clinical responses, ultimately minimizing the burden of cognitive decline on families and healthcare systems. The benefits of using BCIs extend beyond just diagnostics; they also encompass education and patient empowerment, leading to more informed health choices. While challenges remain, the continuous evolution of BCI technology holds immense potential for improving cognitive health management. As researchers and practitioners collaborate to overcome obstacles and refine these tools, a future where cognitive disorders are addressed proactively rather than reactively is becoming increasingly tangible. Society stands at the intersection of technology and healthcare, and embracing BCIs can lead to a better understanding of cognitive health dynamics. Ultimately, brain-computer interfaces may well redefine how we approach cognitive disorders, marking a significant advancement in healthcare and improving the lives of those affected.
To summarize, brain-computer interfaces have ushered in a new era for early detection of cognitive disorders. Therefore, continued research is paramount to harness the power of technology in cognitive health monitoring, education, and treatment. This innovative approach can significantly mitigate the impact of cognitive decline at an individual and societal level. As these technologies are developed and improved, individuals can expect a future where cognitive health is monitored routinely, ensuring timely interventions, support, and rehabilitation as necessary. By embracing these advancements, we encourage a paradigm shift that prioritizes proactive management of cognitive health.