The Connection Between Antibiotics, Gut Flora, and Mood Disorders
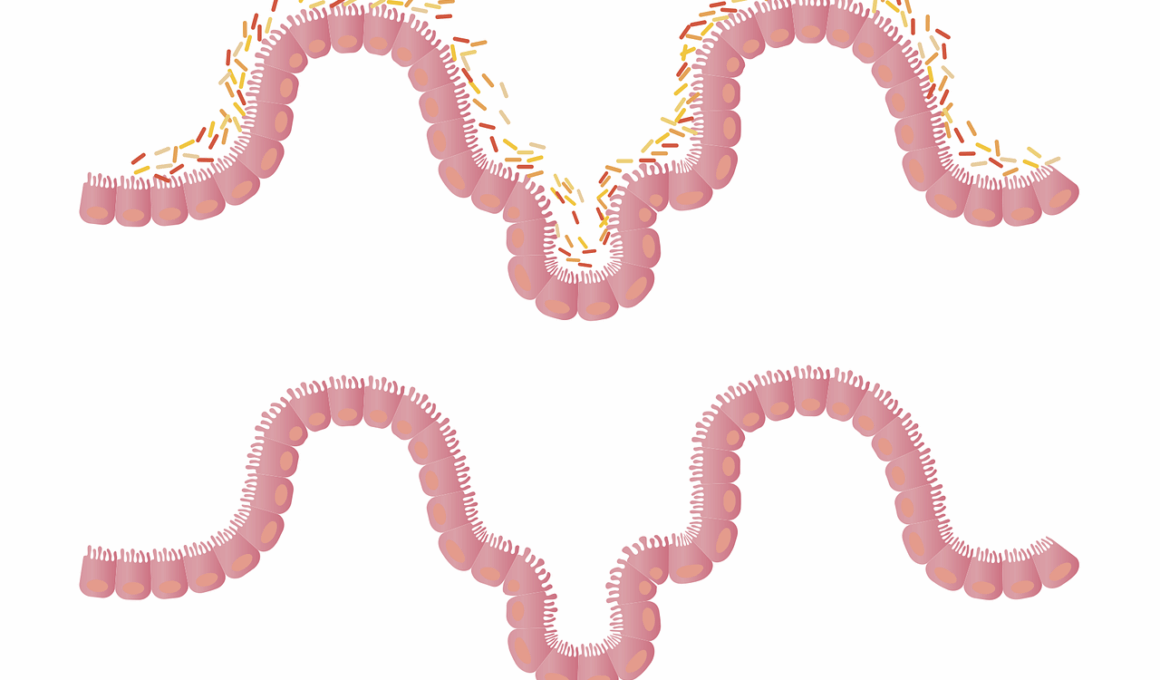
Antibiotics play a crucial role in medicine, fighting bacterial infections effectively. However, their impact on gut flora is noteworthy and comes with potential consequences. Gut flora, or microbiota, consists of trillions of microorganisms that inhabit our intestinal tract. When antibiotics are administered, they can disrupt the delicate balance of these microorganisms, leading to a variety of digestive issues. Disruption can result in an imbalance, leading to the overgrowth of harmful bacteria and a decrease in beneficial bacteria. This shift can cause symptoms like diarrhea, bloating, and abdominal pain. Moreover, gut health is not just about digestion – it drastically influences overall wellbeing. The gut-brain connection is an increasingly studied phenomenon illustrating how gut health affects mental health in significant ways. Studies suggest that changes in gut flora can be linked to mood disorders such as anxiety and depression. Since many neurotransmitters responsible for regulating mood are produced in the gut, it’s essential to maintain a healthy microbiome. To mitigate these adverse effects, alternatives such as probiotics should be explored to restore gut bacterial balance. Furthermore, modifications in diet can help enhance gut health post-antibiotic treatment.
The relationship between antibiotics and mood disorders extends beyond direct effects on gut flora. Research shows that the microbiome influences the body’s inflammatory response. Elevated inflammation levels can directly correlate with depression and anxiety symptoms. When antibiotics disrupt gut flora, they can lead to increased inflammation and alter the gut-brain axis. Additionally, certain species of gut bacteria are known to produce vital neurotransmitters, such as serotonin, which plays a crucial role in mood regulation. If these bacteria are diminished due to antibiotic use, the production of serotonin may be decreased, contributing to mood imbalances. This might explain why some individuals report experiencing mood changes following antibiotic treatment. Moreover, prolonged antibiotic use can contribute to systemic dysbiosis, thus exacerbating pre-existing mental health issues. A study highlighted a correlation between antibiotic prescriptions and greater incidences of psychiatric disorders. Understanding this connection is integral to the treatment of bacterial infections, and clinicians should consider the broader implications of antibiotic use. It becomes increasingly important to evaluate the risks associated with the use of antibiotics, particularly in patients with a history of mood disorders.
Recovery Strategies for Gut Health
To counter the negative impacts of antibiotics on gut flora and mental health, recovery strategies must be implemented promptly after antibiotic treatment. First, incorporating probiotics into the diet is beneficial. Probiotics can restore the balance of good bacteria in the gut. Fermented foods like yogurt, kefir, sauerkraut, and kimchi are excellent sources of probiotics that can promote intestinal health. Additionally, prebiotic foods can help by providing the necessary nutrients for beneficial gut bacteria to thrive. Foods rich in fiber, such as fruits, vegetables, and whole grains, can effectively nourish these beneficial bacteria. Another recovery method is to stay hydrated and ensure adequate water intake. Proper hydration aids digestion and fosters optimal gut function. Moreover, dietary modifications should ensure a low-sugar and low-processed food intake, as high sugar intake can promote the growth of harmful bacteria. Regular physical activity is also crucial for maintaining gut health. Exercise helps stimulate gut motility and encourages the diversity of gut microbiota. Lastly, manage stress levels through practices like mindfulness and yoga, as stress can significantly impact gut health and overall mental wellbeing.
Another important factor related to antibiotics and gut health is the timing and dosage of antibiotic use. Research has revealed that not all antibiotics impact gut flora equally; some can disturb the microbial environment more severely than others. Thus, a clinician’s choice of antibiotic should consider its potential consequences on the microbiome, ultimately affecting mood and mental health. Short courses of narrow-spectrum antibiotics may minimize perturbations in gut flora compared to broad-spectrum antibiotics used for extended durations. It’s imperative for healthcare providers to communicate the gastrointestinal side effects to patients clearly. Awareness can help patients understand the importance of restoration after treatment, stressing the necessity of following up with a healthcare provider tailored to their needs. Emphasizing diet and lifestyle changes post-antibiotic therapy can also empower patients to take charge of their gut and mental health. Additionally, future research into individualized treatments and the development of targeted antibiotics which limit microbial disruption is necessary. Scientists are exploring alternatives that could provide effective bacterial infection treatments without hindering gut flora integrity, thus preserving mental health.
The Role of Diet in Gut and Mental Health
Diet plays a pivotal role in the health of gut microbiota and thereby influences mental health. Incorporating a diet that nurtures the gut is essential, particularly after antibiotic treatment. Highly processed foods and those rich in sugars can be detrimental, as they may lead to dysbiosis and inflammation, potentially worsening mood disorders. Focus on consuming a variety of plant-based foods to maintain a healthy gut environment. These foods are typically high in fiber, nourishing beneficial bacteria, and promoting diversity in the gut microbiome. Essential fatty acids found in fish, nuts, and seeds also contribute positively, as they help reduce inflammation throughout the body. Additionally, antioxidants present in fruits and vegetables have protective effects against oxidative stress, which is linked to depression. Supplementing the diet with omega-3 fatty acids may further enhance mood stabilization. Some studies suggest that a Mediterranean diet may offer protective benefits against depression, linking diverse bacteria populations to better mental health outcomes. Ultimately, adopting a whole-foods-based nutrition plan can greatly improve gut flora, contributing to better emotions and overall health balance.
As researchers continue to explore the gut-brain axis, they are uncovering complexities in how gut flora affects mood and mental health. Emerging studies indicate that the microbiome communicates with the brain via the vagus nerve and through the production of neurotransmitters. This suggests that restoring gut flora could have powerful implications for mood disorders. Furthermore, studies on the use of prebiotics and their effects on mental health are promising. Prebiotics, such as inulin and oligosaccharides, can enrich beneficial bacteria, potentially improving brain function and mood. While this area of study is in its infancy, preliminary findings are encouraging. Future clinical trials will be vital in pinpointing effective interventions combining dietary, psychobiotic, and psychological approaches to treating mood disorders post-antibiotic. Increased awareness of the importance of gut health and its links to mental health can lead to better treatment options. Moreover, health professionals should consider its ramifications when working with patients, particularly those experiencing mental health issues following antibiotic use. Building awareness about these connections can foster a more integrated approach to healthcare.
Conclusion
In conclusion, the relationship between antibiotics, gut flora, and mood disorders is intricate and multifaceted. Understanding how antibiotics affect gut microbiota and subsequently impact mental health is vital for holistic medical practices. With the right recovery strategies, including a diet rich in probiotics and prebiotics, individuals can take actionable steps towards restoring their gut health. As ongoing research evolves, it is crucial for clinicians and patients alike to remain informed about the potential risks and benefits associated with antibiotic treatments. Integrating knowledge from studies on the gut-brain axis into clinical practice can help optimize patient outcomes. Furthermore, the exploration of alternative treatments and dietary modifications, in conjunction with psychological support, will pave the way for comprehensive care tailored to individual needs. The connection between gut health and emotional wellbeing demonstrates that sustaining a healthy microbiome is an essential component of mental health. Healing from antibiotic use entails not merely addressing physical symptoms but considering the broader context of mental well-being as well. A proactive approach in monitoring gut health following antibiotics can significantly benefit individuals both physically and mentally.
In this exploration of gut health, antibiotics, and mood disorders, it is evident that our approach must evolve. By recognizing the profound impact gut flora has on mental health, practitioners can adjust their treatment protocols. Antibiotics, while lifesaving, do not come without their consequences, and patient education is crucial. Promoting discussions around gut health during medical consultations and encouraging lifestyle changes can lead to healthier outcomes. As our understanding deepens, we hope to see an era where restorative treatments are the norm following antibiotic therapy. Moreover, a societal shift towards valuing gut health will encourage better dietary practices. Advocating for research to better understand individual responses to antibiotics and gut flora dynamics is essential for future advances. Thus, we can ensure that mental health is prioritized alongside physical healing, creating a synergistic approach to patient care. The journey toward complete well-being should encompass all facets of health. Furthermore, sustaining this knowledge will contribute to the evolution of evidence-based practices, significantly improving public health outcomes. By fostering collaboration between healthcare providers and patients in promoting gut health, we will enhance quality of life and overall satisfaction in healthcare experiences.