The Economic Impact of Weight on Chronic Disease Management
Weight management has become an increasingly critical public health issue in relation to chronic diseases. This nexus significantly influences healthcare costs and economic productivity. Chronic diseases such as diabetes and heart disease are not only burdensome on affected individuals but also on the healthcare systems globally. As the prevalence of obesity rises, so do associated complications, leading to increased healthcare spending. Studies indicate that individuals with obesity have medical expenses that are approximately $1,400 higher annually than their normal-weight counterparts. The financial implications extend beyond personal expenses; they affect employer costs through increased health insurance premiums and lost productivity due to absenteeism. Effective weight management not only mitigates chronic disease risks but also contributes positively to economic health by reducing these burdens. Addressing weight-related health issues requires a multifaceted strategy that incorporates policy changes, community-based initiatives, and personal responsibility. Governments and organizations must collaborate to promote wellness. Encouraging a healthier lifestyle can decrease the incidence of chronic diseases, resulting in considerable economic savings. This urgent matter calls for enhanced awareness on how weight management is pivotal in tackling chronic diseases and their economic consequences.
Factors influencing weight management are crucial in understanding the prevalence of chronic diseases. Lifestyle choices, genetic predisposition, and socio-economic status play significant roles. Individuals often overlook the importance of diet and exercise, which are vital components in controlling weight. Poor nutritional habits combined with sedentary lifestyles create a recipe for obesity, influencing the onset of chronic diseases. Education around healthy eating options and regular physical activity must be prioritized to reverse this trend. Public health campaigns focusing on these aspects have begun to gain traction but require more widespread implementation. Furthermore, access to healthy food options is often unequal, leading to disparities in health outcomes. Rural and low-income urban communities frequently lack resources for nutritious foods, exacerbating the prevalence of obesity and its related conditions. Improving community infrastructure for health can lead to better outcomes. These initiatives could include making healthy food accessible and affordable to everyone. Slowly but surely, transforming community health requires ongoing commitment. Investing in these lifestyle changes not only improves individual health but also reduces overall economic burdens associated with chronic diseases.
Healthcare Costs and Economic Burden
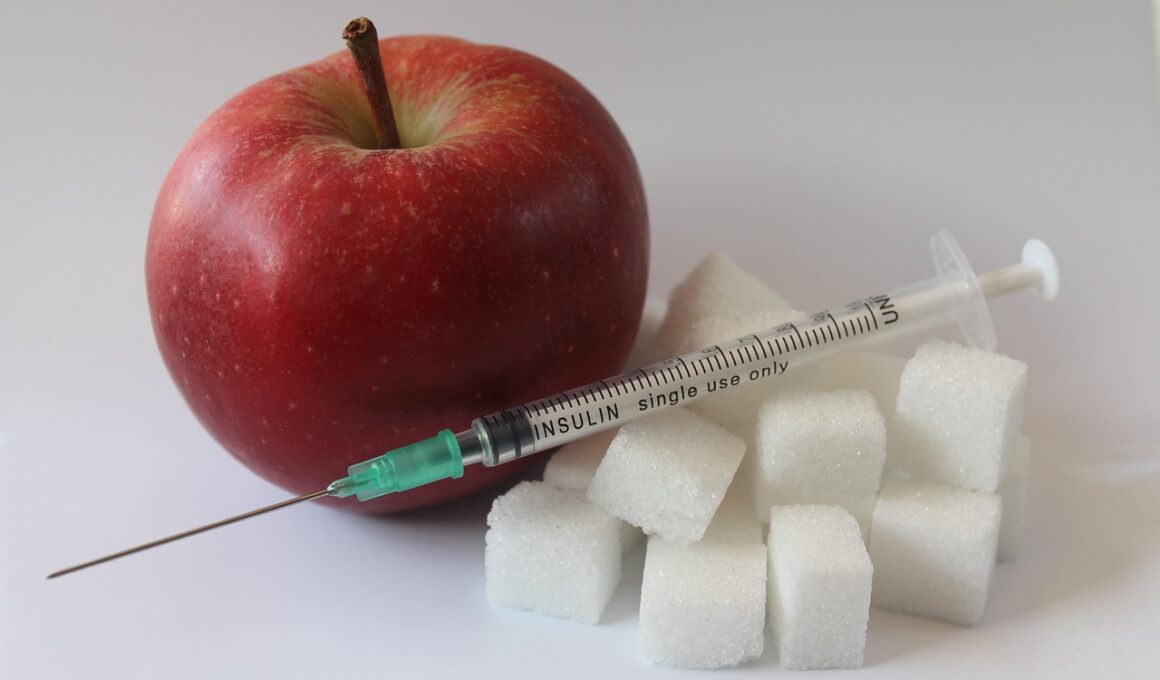
The healthcare costs associated with chronic diseases related to obesity are staggering. Research has shown that treating chronic diseases can drain significant financial resources from families and healthcare systems. With rising obesity rates, health conditions such as hypertension, type 2 diabetes, and heart diseases continue to create a looming crisis. The Centers for Disease Control and Prevention (CDC) estimates that obesity-related health care costs totaled $147 billion in 2008 alone, a figure that has undoubtedly increased. These costs stem from direct medical expenses like hospital stays and indirect costs such as lost wages and reduced productivity. The economic burden is disproportionately shouldered by public healthcare systems, but private insurers also feel the strain. Companies face skyrocketing health insurance premiums and increased claims from employees suffering chronic conditions exacerbated by obesity. Moreover, organizations may lose competitive edge due to high employee turnover and absenteeism related to chronic diseases. Therefore, fostering a healthier workforce can yield substantial economic gains. By focusing on preventive measures to manage weight, both individuals and organizations can help decrease these healthcare costs, creating a win-win scenario.
Investing in preventive health initiatives is essential for curtailing the economic repercussions associated with chronic diseases linked to obesity. Preventive programs focusing on community health and personal health education can lead to substantial cost savings. Evidence shows that every dollar spent on preventive care can yield a return of approximately $3.60 in reduced healthcare costs. Community programs focus on promoting healthier lifestyles, making a direct impact on mitigating chronic diseases’ effects. Such interventions include offering free health screenings, nutritional workshops, and fitness challenges. Furthermore, policy changes that encourage active living, such as improved walking paths and access to recreational facilities, contribute significantly to community health. Employers also play a role in promoting these initiatives by supporting workplace wellness programs. By fostering a culture of health within organizations, employees become more engaged and productive. Access to resources for ideal weight management can enhance overall job satisfaction. As the workforce becomes healthier, the benefits transcend personal wellbeing, contributing to broader economic stability. Emphasizing these programs will lead to impressive reductions in the economic impact of chronic diseases associated with poor weight management.
Government and Stakeholder Roles
The roles of government and stakeholders are pivotal in strategizing effective weight management solutions. Public policies play an essential role in shaping community health outcomes. By planning initiatives that promote healthy living environments, governments can set the stage for better management of weight. Schools, in particular, must be included in these policies, providing children with education on nutrition and physical activity. It is also paramount that governments regulate food marketing, especially to children, aiming to minimize the promotion of unhealthy foods. Stakeholders, including healthcare professionals, community organizations, and businesses, have the opportunity to collaborate on initiatives promoting healthier lifestyles. Comprehensive strategies involve engaging these stakeholders through partnerships that combine resources, education, and advocacy. Additionally, insurance companies can incentivize weight management practices by reducing premiums for healthier lifestyle choices. The collective efforts of various players within the community will create a supportive environment that ameliorates the challenges faced. As each stakeholder takes responsibility, the burden of chronic diseases linked to poor weight management can gradually decline. Through cooperation, these entities increase the likelihood of achieving sustainable solutions.
Furthermore, technology continues to advance the field of weight management, enhancing chronic disease prevention efforts. Innovations such as mobile health apps enable users to monitor their weight and establish healthier habits efficiently. These platforms often provide educational resources regarding nutrition and exercise, offering personalized feedback to users. The rise of telehealth services presents additional support, allowing individuals to consult healthcare professionals without leaving their homes. This accessibility can encourage more individuals to seek assistance in managing their weight. Wearable devices tracking physical activity and essential health metrics also contribute positively to weight management efforts. By integrating these technologies into daily life, individuals may find it easier to commit to achieving their goals. Moreover, leveraging social media can amplify the impact of health campaigns aimed at promoting healthier lifestyles. Engaging content can inspire communities to cultivate a culture supportive of weight management initiatives. However, disparities in access to these technologies should be considered. Investing in technology that ensures equitable access helps mitigate existing health disparities. As these approaches gather momentum, they will likely play a significant role in addressing chronic diseases connected to weight. A multi-faceted approach will be vital in driving lasting change.
Conclusion: A Call to Action
In conclusion, the economic impact of weight on chronic disease management demands immediate attention. Addressing this challenge goes beyond individual responsibility; it requires coordinated efforts by governments, healthcare providers, employers, and individuals alike. By highlighting the financial strains associated with chronic diseases, a shared understanding of the urgency can foster collaboration. Creating environments that promote healthy lifestyles has become a necessity. Communities must be at the forefront in designing policies that support weight management. Employers should also prioritize wellness initiatives, as a healthier workforce has proven economic benefits. More importantly, raising awareness about the complexities of managing weight and its connection to chronic diseases is essential. Initiatives aimed at education can empower individuals to make informed choices regarding their health. By fostering community engagement and support networks, the burden of chronic diseases can be alleviated. The path forward lies in pursuing innovative strategies that integrate technology, stakeholder collaboration, and preventive health measures. It is time for all entities involved to advocate for sustainable solutions, leading to improved health outcomes and reduced economic impact. Only through concerted action can we mitigate the repercussions of poor weight management on chronic diseases.
As we embrace the journey towards healthier living, it is crucial to consider the collective efforts necessary for weight management and chronic disease prevention. This multifaceted approach requires action, commitment, and collaboration at all levels. Through informed decisions, sustainable practices, and community support, we can drive positive change in addressing these pressing health concerns. The future of our communities depends significantly on how we tackle this issue. A strong emphasis on preventive health will undoubtedly lead to considerable improvements in overall community health and economic well-being.