The Role of Fasting in Reducing Gut Dysbiosis
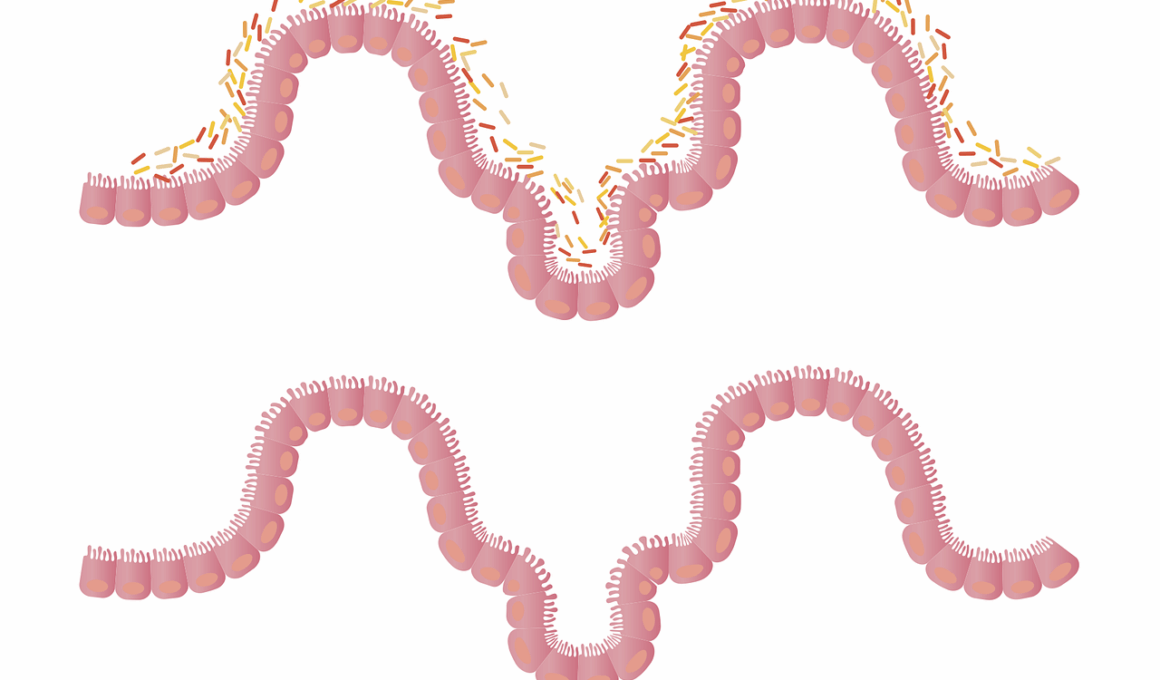
Fasting has become a popular practice for various health benefits, including weight control and improved metabolic processes. Recent studies suggest that fasting can significantly affect gut health, more specifically the gut microbiome. The gut microbiome consists of diverse bacteria that play critical roles in digestion, immune system function, and overall health. Dysbiosis refers to an imbalance of these microorganisms, leading to health issues. Fasting may promote a more balanced gut microbiome by reducing inflammation and allowing beneficial bacteria to flourish. By abstaining from food, the body enters a state where it utilizes existing energy stores, which may positively influence microbial diversity. Potentially beneficial bacteria, such as Bifidobacterium and Lactobacillus, may thrive when fasting is practiced regularly. However, the mechanism behind these changes remains an area of ongoing research. One hypothesis is that fasting leads to alterations in gut pH and nutrient availability, which favor specific microbial populations. In summary, fasting may contribute to reducing gut dysbiosis and promoting overall gut health by fostering balance among bacterial species.
The Mechanisms Behind Fasting and Microbial Balance
Understanding the mechanisms by which fasting influences the gut microbiome is vital for utilizing its benefits effectively. Firstly, fasting may enhance gut permeability, which improves nutrient absorption. When the digestive system is not focusing on processing food, it can allocate resources toward healing and balancing gut bacteria. Additionally, fasting reduces the frequency of meals, which can lower inflammation levels in the gut while promoting beneficial microbes. Another mechanism involves autophagy, a process where cells clear out damaged components. This cellular “clean-up” allows for better gut health, as it may enable the regeneration of cells that support a healthy microbiome. Caloric restriction, often associated with fasting, may further promote microbial diversity by favoring the growth of beneficial bacteria over harmful strains. Moreover, gut hormones fluctuate during fasting, impacting microbiota composition. These hormonal changes can encourage the growth of commensal bacteria while inhibiting pathogens. Studies have shown that these shifts positively correlate with improved metabolic health, contributing to a healthier, more balanced gut microbiome crucial for reducing dysbiosis.
Investigating the relationship between fasting and gut microbiome diversity offers exciting insights into potential health outcomes. Research indicates that a diverse gut microbiome is crucial for optimal metabolic health. A balanced gut microbiome functions efficiently, aiding digestion and nutrient absorption while supporting the body’s immune system. Conversely, dysbiosis can result in metabolic disorders, obesity, and other chronic diseases. Fasting schedules, such as intermittent fasting, have revealed promising results in enhancing microbial diversity. For example, individuals who practice intermittent fasting have shown significant increases in beneficial bacteria populations compared to those who do not. These changes can help redefine the body’s metabolic state, improving responses to insulin and promoting healthy weight maintenance. Alterations in gut microbiota composition have been directly linked to enhanced insulin sensitivity. This implies that fasting not only addresses weight but also addresses the underlying microbial factors contributing to metabolic issues. Accordingly, encouraging people to consider fasting as part of their lifestyle may offer a dual perspective of both physical and microbial improvements.
The Impact of Different Fasting Methods on Gut Health
Various fasting methods can influence the gut microbiome in differing ways, with practices like intermittent fasting, prolonged fasting, and time-restricted eating gaining popularity. Intermittent fasting typically involves cycling between eating and fasting periods, which can foster beneficial gut bacteria while reducing the prevalence of harmful species. By restricting eating windows, individuals may experience more significant microbial shifts compared to traditional dietary habits. On the other hand, prolonged fasting — involving extended periods without food — can lead to dramatic changes in gut biodiversity. Studies suggest that long-term fasting can create conditions that support the growth of beneficial gut microorganisms, as the absence of constant food intake reduces competition. Time-restricted eating aligns eating patterns with circadian rhythms, potentially yielding improvements in gut health. Each method promotes distinct physiological responses, leading to various effects on microbiome composition. Individual responses to fasting techniques can vary greatly based on pre-existing gut health conditions. Therefore, personalizing fasting practices could maximize gut health benefits and mitigate dysbiosis for best results.
The relationship between fasting and mental well-being, along with gut health, is a connection fostering growing interest. The gut-brain axis illustrates how the gut microbiome influences mental health through the production of neurotransmitters. Fasting can enhance gut health, indirectly benefiting psychological states. As fasting promotes microbial diversity and reduces inflammation, researchers hypothesize that it may play a role in decreasing symptoms of anxiety and depression. By modulating neurotransmitter production, the microbiota could influence mood regulation and stress responses. Furthermore, when individuals practice fasting and observe improvements in their overall gut health, they might also experience enhanced emotional wellness. This emphasizes the importance of adopting holistic approaches to health, where fasting serves as an accessible mechanism to improve both gut microbiome balance and mental health. However, it remains essential to approach fasting knowledgeably, as improper practices can lead to adverse outcomes. Consulting healthcare professionals prior to making significant dietary changes ensures that individuals can harness the full benefits while minimizing risks associated with fasting.
Fasting, Lifestyle Changes, and Long-term Effects on Gut Dysbiosis
Incorporating fasting into a balanced lifestyle can yield long-term benefits for gut health. Research suggests that regular fasting can have cumulated effects that lead to sustainable improvements in the gut microbiome. It is important for individuals to pair fasting with nutritious food choices during eating periods, as the overall quality of food plays a crucial role in microbial health. Whole foods, rich in fiber and nutrients, support the growth of beneficial gut bacteria, making them essential partners to fasting. Additionally, hydration is vital, as the gut requires adequate water intake for optimal function. Regular physical activity also promotes a healthy gut microbiome, making it essential to integrate exercise with fasting. Individuals should consider fasting not just as a short-term health intervention but as a long-term lifestyle component. Embracing lifestyle changes can create a more balanced microbiome, reducing dysbiosis and improving overall health. Continued research in this area promises to unravel the complexities of the gut microbiome and its relationship with fasting, ultimately providing tailored approaches for individuals striving for improved health.
In conclusion, fasting appears to play a critical role in mitigating gut dysbiosis and enhancing overall gut health. As research continues to shed light on the intricate relationship between fasting and the gut microbiome, the implications become clearer. The promotion of beneficial bacteria through fasting methods signifies potential therapeutic interventions for various health conditions tied to gut imbalance. Future investigations are necessary to establish specific fasting protocols that yield the best outcomes for individuals with gut dysbiosis. With increasing awareness and multifaceted approaches, incorporating fasting into one’s lifestyle holds promise for long-term health improvements. Individuals considering fasting should aim for informed decisions about their dietary practices, ensuring they prioritize both short-term results and sustainable health benefits. As the connection between gut and mental health is explored further, the broader implications of fasting may lead to enhanced emotional well-being. Therein lies the importance of adopting comprehensive wellness strategies that integrate fasting as a tool, ultimately empowering individuals in their journey toward balanced health and well-being.
Final Thoughts on Fasting and Gut Health
As the scientific community investigates the benefits of fasting, it is clear that this practice offers significant advantages for gut health and gut microbiome balance. Fasting should be approached with mindfulness, recognizing personal health contexts. For those struggling with gut dysbiosis or seeking to optimize their gut health, fasting could serve as an effective strategy. In conjunction with balanced nutrition, hydration, and lifestyle practices, fasting may contribute to a healthier, more balanced gut microbiome. Education about the nuances of fasting methods is essential for maximizing benefits. Individuals must approach each fasting method with an understanding of its unique effects on gut health. Continued research will unveil further connections between fasting, gut microbiome dynamics, and overall health. Ultimately, fasting presents an exciting area of exploration, where emerging science may guide individuals toward healthier lifestyles. By integrating fasting practices thoughtfully, we contribute to a more holistic and health-oriented approach to well-being. Individuals can embrace fasting as a lifestyle choice, cultivating a healthier relationship with food impacted by a balanced gut microbiome.