Resistance Training to Improve Function in Parkinson’s Disease
Parkinson’s Disease (PD) is a progressive neurological disorder that primarily affects movement, causing tremors, rigidity, and balance issues. Engaging in resistance training can significantly enhance function in individuals diagnosed with this disease. Strength training incorporates resistance to stimulate muscle contraction, promoting increased strength and mass. Research indicates that resistance training benefits not only muscular strength but also functional outcomes. Improved muscle strength aids in reducing fall risks associated with Parkinson’s, making everyday activities safer. Strength training can be tailored to the individual’s capabilities, ensuring it is both effective and safe. Therefore, individuals with PD often feel empowered to engage in their rehabilitation, thus enhancing quality of life. Moreover, adherence to a resistance training program offers psychological benefits such as improved mood and enhanced mental well-being. It is crucial for individuals with Parkinson’s to consult healthcare professionals before engaging in any exercise program. A qualified trainer can personalize the regimen to the individual’s needs while ensuring safety and effectiveness. Ultimately, resistance training emerges as a vital component of an exercise regimen tailored for managing Parkinson’s Disease and improving overall functional capabilities.
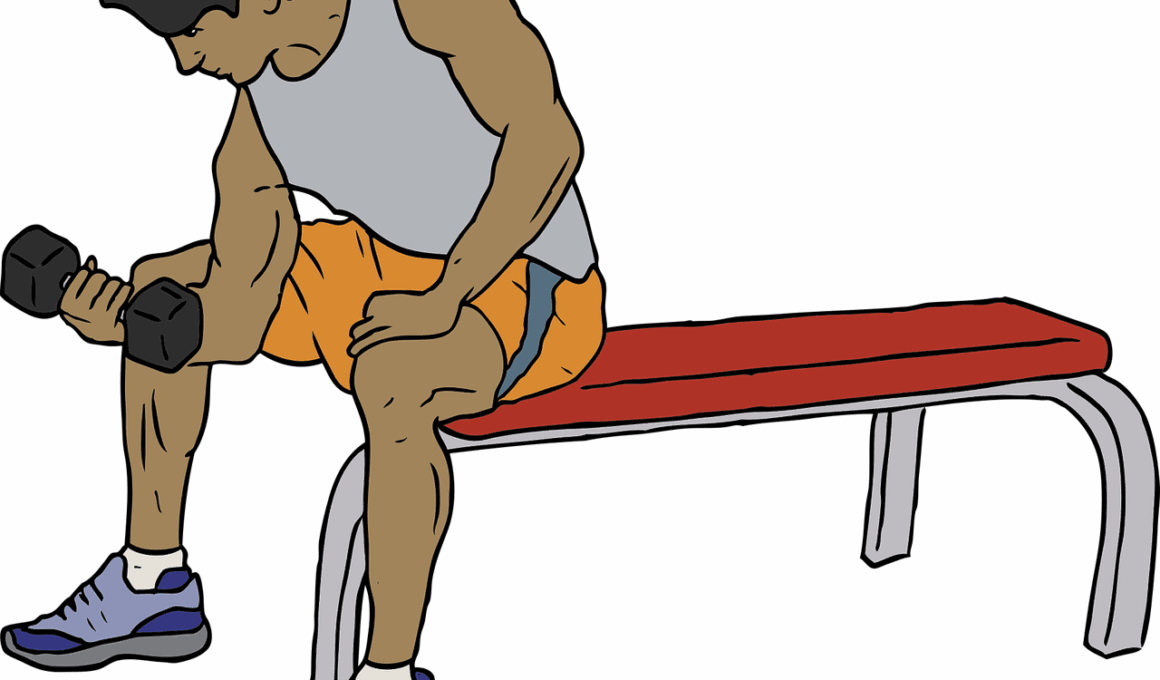
The Benefits of Resistance Training
Resistance training offers multifaceted benefits for individuals suffering from Parkinson’s Disease, aiding in the improvement of muscle strength, balance, and flexibility. Regular participation in strength training may counteract the muscle atrophy and weakness associated with PD. Enhanced muscle strength contributes to improved overall functional mobility, allowing patients to perform activities of daily living with greater ease. Furthermore, studies show that resistance training can address the motor deficits often experienced by those with Parkinson’s. This ultimately helps improve gait mechanics and stability, reducing the likelihood of falls. Importantly, improved muscle strength also correlates with the increased capacity for physical activity, empowering individuals to engage more actively in their lives. Additionally, participants often experience improvements in confidence and self-efficacy as they witness the progression in their strength and abilities. Incorporating functional exercises into training routines further enhances the positive impact of strength training. It bridges the gap between exercise and everyday life functions. Therefore, strength training emerges not just as a therapeutic strategy but also as a tool for enhancing the overall quality of life and independence for those battling Parkinson’s Disease.
To understand the effectiveness of resistance training in Parkinson’s Disease, it is crucial to incorporate a structured exercise program that adheres to the individual’s progression. A well-designed program typically includes a variety of exercises that focus on major muscle groups as well as functional movements. Duration and intensity can be gradually progressed based on individual tolerance and skills, ensuring safe advancements. Practicing resistance training approximately two to three times weekly can optimize benefits while minimizing discomfort and risk of injury. Moreover, using both machine-based and free weight exercises diversifies the training program, making it more engaging and comprehensive. Moreover, flexibility exercises should be included to promote a full range of movement capability. As the individual grows stronger, the incorporation of balance and coordination exercises will further support the functional capabilities of those with Parkinson’s. Individuals training under professional supervision tend to adhere better to these programs, generally achieving superior results. Consistency with resistance training fosters incremental improvements in overall health and functionality. Thus, the commitment to a structured strength program offers individuals with Parkinson’s valuable skills for enhancing their autonomy and quality of life through targeted exercises and functional training.
Safety Considerations During Resistance Training
When implementing resistance training for individuals with Parkinson’s Disease, safety remains a top priority. It is crucial to assess each patient’s health status prior to initiating an exercise program. Healthcare providers can help identify limitations and medical considerations to tailor a safe exercise approach. Key factors include monitoring blood pressure and heart rate before and after exercise sessions. It is also essential to create a supportive environment to minimize the risk of falls during strength training exercises. Appropriately selecting exercise equipment that is easy to handle and stable contributes as well. Practitioners should educate patients on proper lifting techniques and providing necessary equipment adjustments to avoid injuries. The strength exercises should commence at a manageable intensity, gradually increasing as proficiency and comfort grow. Additionally, regular feedback on techniques and performance can significantly reduce injury risks. Focusing on correct form and movement will cultivate a safer and more effective training atmosphere. Encouragement from trainers and healthcare providers can motivate individuals with Parkinson’s to engage in resistance training, making them more likely to adhere to their exercise programs. Therefore, understanding and addressing these considerations is vital in achieving desired outcomes safely.
Progress monitoring in resistance training programs is essential to evaluate the effectiveness of interventions applied to individuals with Parkinson’s Disease. Regular assessments provide valuable insights into patients’ improvements in strength, endurance, and functional outcomes. Healthcare professionals can set realistic short-term and long-term goals aligned with the individual’s needs and abilities. Adapting the training regimen based on progress will ensure continued engagement and satisfaction with the program. Utilizing outcome measures consistently allows trainers to fine-tune techniques, ensuring the exercises remain appropriately challenging while preventing plateaus. Typically, reassessing strength and functional performance every few weeks is advisable. This not only tracks improvements but also establishes accountability, motivating patients to remain active participants in their rehabilitation. Feedback regarding progress encourages adherence and helps define future training goals. Encouraging patients to maintain a training log can facilitate individual reflection on improvements. Ultimately, frequent assessments foster motivation and engagement, allowing patients to experience the tangible benefits of their efforts in real-time. Therefore, effective monitoring of resistance training in Parkinson’s Disease paves the way for sustained improvements and enhances overall well-being.
Community and Support for Individuals with Parkinson’s
Community support plays a vital role in the lives of individuals living with Parkinson’s Disease. Engaging in group exercise sessions not only enhances motivation but also fosters social interaction among participants. Peer support groups create a strong sense of belonging, providing reassurance and encouragement during recovery journeys. Connection with others facing similar challenges empowers individuals to share experiences, techniques, and goals. Further, trainers with expertise in Parkinson’s care can facilitate knowledgeable exercise sessions tailored to this unique population. Many local health clubs, community centers, and nonprofit organizations offer inclusive exercise programs or classes designed for individuals with PD. These classes emphasize strength training, flexibility, and balance while fostering a supportive community atmosphere. Additionally, bringing family members into the training process can encourage a healthier environment and ensures compliance outside of structured sessions. Virtual communities provide alternatives for individuals unable to attend in-person classes, utilizing online platforms for shared experiences, resources, and support. Ultimately, participation in community exercises fosters personal connections while enhancing physical health through resistance training tailored for the unique needs of those living with Parkinson’s. Lives can be transformed through collaboration and support.
In conclusion, resistance training has striking potential in improving functionality and quality of life for those living with Parkinson’s Disease. The incorporation of structured resistance training programs focused on strength and mobility helps patients to maintain autonomy and remain active participants in their everyday lives. Emphasizing safety, continuous support, and proper assessment are vital components to successful outcomes. Mental and emotional benefits also arise when individuals find empowerment through strength training, enhancing their overall well-being. The collaborative efforts of trainers, healthcare providers, and community support bolster adherence to exercise regimens. Ongoing research will continue to elucidate and refine effective strategies for incorporating resistance training into the comprehensive management of Parkinson’s. Consequently, training positively impacts not only physical health but affects social and emotional aspects of patients’ lives. Patients learning about their strengths through resistance work will likely feel more invested in their rehabilitation journey. Implementing these exercise protocols can create transformative change, demonstrating that individuals with Parkinson’s can enjoy improved functional outcomes, independence, and quality of life. Therefore, acknowledging the invaluable contributions of resistance training culminates as a beneficial alternative for managing chronic conditions such as Parkinson’s Disease.