Research Advances in Gut Microbiome and Type 2 Diabetes
The gut microbiome plays a pivotal role in the overall health and well-being of individuals. Recent research has highlighted its significant influence on various metabolic disorders, particularly Type 2 Diabetes. Studies suggest that gut bacteria composition can affect insulin sensitivity, glucose metabolism, and inflammation, thereby paving the way for potential new approaches to prevention and treatment. For instance, a diverse microbiome is believed to improve the gut barrier function, which may reduce systemic inflammation and metabolic dysregulation associated with diabetes. Investigating the gut-brain axis further emphasizes how microbial communities can modulate hunger and satiety, impacting weight gain and metabolic health. Thus, improving gut health through dietary interventions may assist in managing or preventing Type 2 Diabetes. Furthermore, the identification of specific microbial strains that benefit glucose metabolism could lead to personalized probiotic therapies. Future research aims to create robust clinical guidelines for leveraging these findings and integrating them into standard diabetes care. This could revolutionize the treatment landscape and offer new hope for individuals struggling with this increasingly prevalent condition. As understanding of the gut microbiome deepens, its integration into clinical practice becomes more promising.
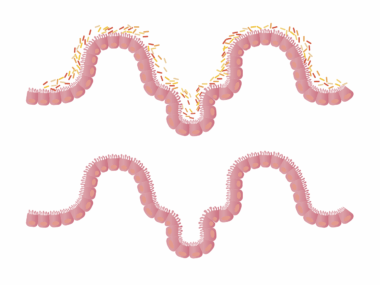
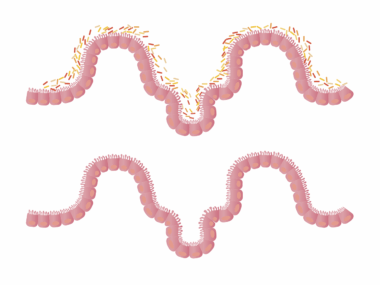
One significant area of focus has been the relationship between gut microbiota and inflammation. Researchers have consistently found that chronic low-grade inflammation is a key player in the development of Type 2 Diabetes. This inflammation can arise from an imbalance in gut bacteria, commonly referred to as dysbiosis. A less diverse gut microbiome often leads to an overgrowth of harmful bacteria, which can trigger inflammatory responses. Recent meta-analyses have linked specific bacterial genera, such as Firmicutes and Bacteroidetes, to insulin resistance and metabolic syndrome. To mitigate inflammation and restore microbial balance, interventions such as dietary changes or the use of probiotics are being explored. Studies evaluating high-fiber diets, for instance, show promise in promoting beneficial microbiota, which could enhance insulin sensitivity. Clinical trials are being conducted to assess how manipulating the gut microbiome through prebiotic supplementation can influence metabolic health markers. Simultaneously, the potential of leveraging these insights to tailor individualized diets for better glycemic control creates a pathway towards personalized nutrition and diabetes management. As findings evolve, they contribute to the larger discourse on lifestyle changes necessary for combating diabetes effectively.
The role of dietary patterns in shaping gut microbiome health and, subsequently, Type 2 Diabetes outcomes cannot be understated. A growing body of evidence suggests that certain dietary choices can exert profound effects on gut microbial composition. For instance, Mediterranean-style diets rich in vegetables, fruits, whole grains, and healthy fats have been associated with improved microbiome diversity and lower diabetes risk. Conversely, diets high in sugars and processed foods promote dysbiosis, adversely affecting metabolic health. Research emphasizes the importance of polyphenols and fiber in promoting beneficial gut bacteria while suppressing pathogenic strains. Longitudinal studies measuring dietary intake against gut microbiome data have revealed that consistent adherence to a plant-based diet leads to more favorable outcomes. However, it’s not just about what is consumed but also about how food is prepared. Fermented foods, in particular, have shown potential in enhancing gut health. Therefore, increasing awareness and education about the impact of diet on the gut microbiome is essential for public health initiatives. Shifting societal norms towards embracing healthier eating habits may hold significant promise in curbing the diabetes epidemic as well as various other lifestyle diseases.
The Gut–Brain Connection and Diabetes
Another fascinating aspect of the gut microbiome’s role in Type 2 Diabetes is its connection to the brain. The gut-brain axis represents bidirectional communication between the gastrointestinal tract and the central nervous system. Recent studies indicate that microbial metabolites can influence brain function and, subsequently, appetite regulation. For example, short-chain fatty acids (SCFAs) produced by gut bacteria during fiber fermentation affect neurotransmitter synthesis, which potentially impacts feelings of hunger and satiety. Understanding this connection provides insights into behavioral changes necessary for managing Type 2 Diabetes. Furthermore, chronic stress and psychological conditions can also alter the gut microbiome, creating a vicious cycle that complicates diabetes management. Research has noted that individuals with diabetes often experience increased anxiety or depression, phenomena that may further disrupt gut health. By recognizing the interplay between mental health, gut health, and metabolic conditions, holistic approaches for diabetes treatment could be developed. For instance, mindfulness practices and stress reduction techniques may not only improve mental health but also promote a healthy gut microbiome, making them valuable components of comprehensive diabetes care.
Apart from dietary influences, genetic factors also play a role in determining gut microbiome composition and its relationship with Type 2 Diabetes. Studies involving twin populations show that heredity significantly dictates microbial diversity and abundance, affecting metabolic pathways. Each individual possesses a unique microbiome shaped by genetics, lifestyle, and environmental interactions. Consequently, this uniqueness implies that personalized treatment plans considering an individual’s genetic predispositions could emerge. Researchers are unraveling the genetic underpinnings that could predict which individuals are likely to develop diabetes based on their gut microbiome profiles. Genetic analyses are combined with microbiome sequencing to establish correlations between specific genetic markers and microbiota traits. By employing a precision medicine approach, healthcare providers may be enabled to devise personalized intervention strategies that target the specific microbial deficiencies characteristic of each patient. This methodology not only enhances the effectiveness of interventions but also reduces the risks of side effects associated with generalized treatments. As this field advances, the potential for translating these findings into mainstream therapeutic applications becomes an exciting frontier in diabetes research.
Additionally, emerging technologies in microbiome analysis have revolutionized research and diagnostics in gut health and Type 2 Diabetes. Advanced sequencing techniques now enable researchers to map the human microbiome more accurately than ever before. Metagenomic analyses can identify specific bacterial strains and their functional capacities, offering insights into how these bacteria could influence metabolism and health. This high-resolution profiling allows for a better understanding of potential biomarkers that could predict diabetes risk and progression. Moreover, bioinformatics tools are critical in interpreting complex microbiome data, facilitating the identification of patterns correlating with health outcomes. Such technological advancements pave the way for more comprehensive research designs, including large-scale population studies aimed at understanding the microbiome’s role in chronic diseases. With these improvements in microbiome research methodologies, tracking shifts in microbial diversity in response to interventions becomes feasible. Furthermore, developing point-of-care diagnostic tools to assess gut health could lead to earlier interventions for individuals at high risk of Type 2 Diabetes, ultimately improving patient outcomes and reducing the burden of this widespread disease.
Future Directions in Gut Health Research
Looking towards the future, the landscape of gut health research is ripe with opportunities that could significantly alter management strategies for Type 2 Diabetes. Continued exploration into personalized nutrition and targeted probiotic therapies holds great promise for metabolic health. As we learn more about specific bacterial strains beneficial for blood sugar regulation, the potential exists to develop highly tailored dietary regimens or supplements for at-risk populations. Moreover, the integration of lifestyle modifications, including physical exercise and stress management, into treatment plans could enhance outcomes by synergistically benefiting both mental and gut health. Additionally, as research uncovers the intricate biochemical pathways mediating gut-microbiome interactions, novel pharmaceutical interventions based on these insights could emerge. In parallel, global awareness campaigns could also amplify the importance of gut health in diabetes prevention, identifying effective outreach strategies tailored to diverse populations. Ultimately, fostering multidisciplinary collaborations involving nutritionists, microbiologists, clinicians, and public health experts will facilitate a more comprehensive understanding of the gut’s role in diabetes. As the field progresses, it may unlock significant breakthroughs essential for combating this prevalent health crisis effectively.
In conclusion, the emerging research in gut health signifies a paradigm shift in our understanding of Type 2 Diabetes. The intricate relationship between the gut microbiome and metabolic health reveals new avenues for intervention and treatment. While traditional approaches focus on pharmacological treatments and lifestyle adjustments, integrating gut health into diabetes management could lead to innovative and holistic strategies. The key lies in fostering a healthy gut through tailored dietary choices, maintaining microbial diversity, and addressing underlying inflammatory processes. As scientists delve deeper into the complexities of the human microbiome, personalized medicine based on an individual’s unique microbiome could transform diabetes care. Furthermore, educating the public about the importance of gut health can empower patients, leading to more proactive approaches to managing their health. Recognizing that Type 2 Diabetes is not solely a metabolic disorder but involves complex gut-brain interactions encourages a broader understanding of this phenomenon. Research advances signal an exciting future in the management and prevention of not only Type 2 Diabetes but various lifestyle-related diseases. The evolution of our knowledge in this area will undoubtedly shape public health policies and inform healthcare practices going forward.