Diet Plans That Support Gut Health for SIBO Patients
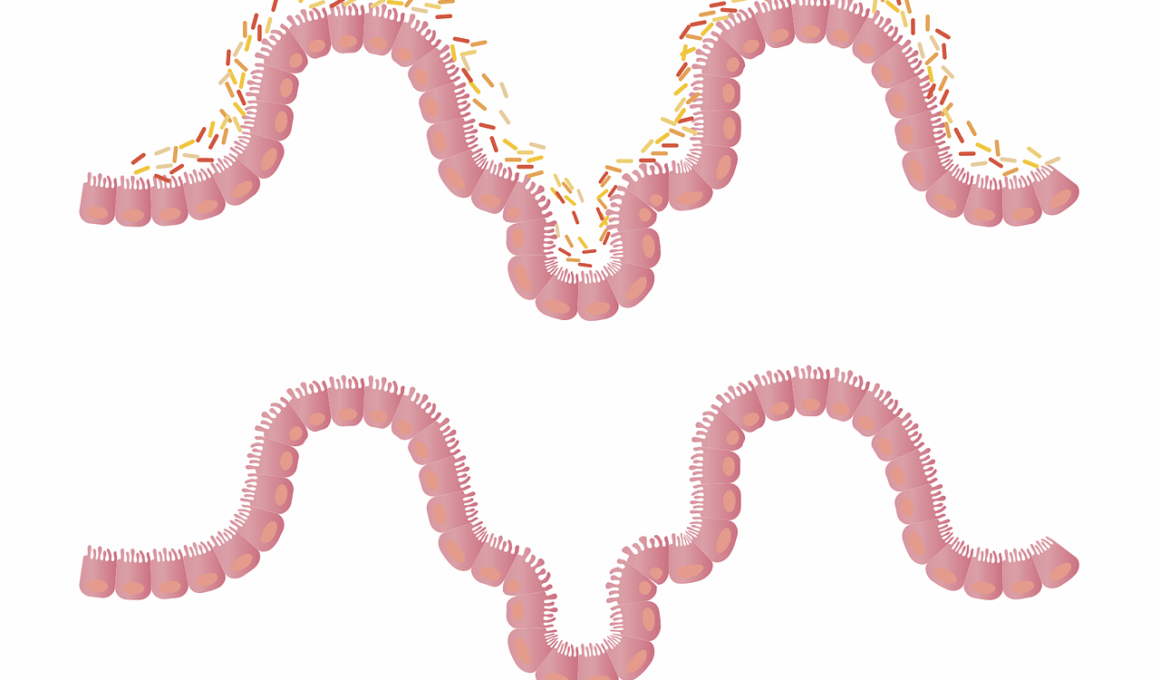
Small Intestinal Bacterial Overgrowth (SIBO) is a digestive condition that can lead to significant discomfort and nutritional deficiencies. Diet plays a crucial role in managing SIBO symptoms and improving gut health. A well-structured diet plan can help reduce bacterial overgrowth and alleviate symptoms such as bloating, diarrhea, and abdominal pain. One of the most effective approaches is the Low Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols (FODMAP) diet. This diet minimizes certain carbohydrates which ferment in the intestines. Consuming easily digestible foods is also essential. Lean proteins, healthy fats, and low FODMAP vegetables should be the main focus. Fermented foods rich in probiotics are often considered beneficial, but caution with SIBO is needed. It’s best to consult a healthcare professional for personalized advice. These dietary modifications might seem daunting, but understanding how specific foods affect the condition allows for better control of SIBO symptoms and overall health improvements. Adhering to these dietary principles may aid recovery from SIBO and enhance one’s quality of life.
Implementing a low FODMAP diet requires careful planning to ensure nutritional adequacy. Foods high in FODMAPs, like wheat, garlic, onion, and certain dairy products, should be eliminated completely at first. Meanwhile, choosing low FODMAP alternatives is paramount. Safe options include rice, quinoa, oats, and gluten-free products. Fruits like bananas, blueberries, and grapes are considered safe, while apples and pears should be avoided. Vegetables such as carrots, spinach, and zucchini make ideal choices. Being mindful about portion sizes is also important, as larger servings of low FODMAP foods could still trigger symptoms. Along with dietary restrictions, maintaining hydration and consuming bone broth or clear soups can provide additional nutrients and hydration. Tracking food intake and symptoms can also be highly beneficial in identifying personal triggers and refining the diet plan. As symptoms improve, reintroducing high FODMAP foods gradually can help determine tolerance levels. Additionally, working with a registered dietitian can assist patients in designing a balanced diet suitable for SIBO management while ensuring they receive all necessary nutrients for recovery and optimal gut health.
Importance of Personalized Nutrition
Personalized nutrition is critical for individuals diagnosed with SIBO because the condition affects everyone differently. While low FODMAP diets offer a general guideline, it is essential to adapt meal plans based on personal tolerance and preferences. Each individual may have distinct responses to various foods, and understanding these differences is key in successfully managing gut health. Some patients might react negatively even to low FODMAP foods in large quantities, necessitating a tailored approach. Keeping a food diary can help track symptoms and identify what works best for maintaining gut health. It’s recommended to address other dietary aspects that could affect the gut microbiome as well. For instance, incorporating anti-inflammatory foods such as ginger and turmeric can provide additional health benefits. Additionally, considering the types of fats consumed matters; healthy oils like olive oil and avocado oil can promote digestive health. Regular consultations with healthcare providers will ensure the diet aligns with improving gut health while addressing all nutritional needs. A person’s diet should evolve as symptoms change, making it vital to remain flexible and attentive to how foods impact individual comfort and overall wellbeing.
Incorporating healthy fats into one’s diet is another essential component for managing SIBO. Healthy fats not only provide essential nutrients but also support absorption because certain vitamins are fat-soluble. Avocado, nuts, seeds, and olive oil are great sources of these healthy fats. They can be easily added to meals, enhancing flavor and nutrient profile. Additionally, fats play a crucial role in maintaining energy levels, especially for those on restrictive diets. It is important to choose fats wisely and avoid processed oils which may contribute to inflammation in the gut. Moreover, supplementation might be necessary to combat deficiencies that arise from restrictive dieting. Seeking support from a healthcare provider to evaluate specific dietary needs can help in restoring a balanced nutritional profile. Probiotic supplements might also be beneficial, but always consult a doctor before starting new supplements. Furthermore, stress management and lifestyle choices should not be neglected. Regular exercise, mindfulness practices, and adequate sleep are crucial elements in supporting overall gut health. Combining all these aspects leads to a holistic approach in dealing with SIBO, improving quality of life and, ultimately, aiding in recovery.
The Role of Hydration
Staying hydrated is often underestimated when it comes to gut health, especially for individuals with SIBO. Proper hydration is critical for digestion and helps regulate the intestinal environment. When the gut is functioning optimally, it can aid in reducing SIBO symptoms. Water plays a crucial role in maintaining digestive motility and can prevent constipation, which may be a side effect of restrictive dieting. Herbal teas and broths can also be beneficial, providing warmth and additional nutrients. Electrolyte balance is essential, as dehydration can exacerbate symptoms. Individuals should aim for at least eight glasses of water daily, adjusting based on physical activity levels. Infusing water with lemon or herbs can enhance flavor and increase water consumption. On the other hand, alcohol and caffeinated beverages may worsen SIBO symptoms and should be limited. When planning meals, pairing foods with adequate fluids helps in the overall digestive process. Hunger cues should be respected, and adequate meal spacing can aid in preventing excess bacteria from populating the small intestine. Attention to hydration needs can transform the dietary experience, making it enjoyable and beneficial for gut health.
Maintaining a balanced intake of fiber is another pivotal aspect of dietary management for SIBO. While some fiber-rich foods are high in FODMAPs and should be avoided, others can be beneficial for gut health. Soluble fiber, found in foods like oats and chia seeds, can help maintain regular bowel movements without exacerbating SIBO symptoms. It’s imperative to gradually increase fiber intake to allow the gut time to adjust. However, the specific type and amount of fiber tolerated can vary widely among individuals, necessitating a personalized approach. Increasing fiber intake too quickly may lead to digestive upset, so careful monitoring is vital. Discussing fiber intake with a nutrition expert can help identify the best options for your needs. Fiber not only aids in digestion but also contributes to overall gut health by feeding beneficial gut bacteria, which is an essential aspect in tackling SIBO. Supplementing with fiber may be beneficial in some cases, providing added support to help alleviate symptoms. Ultimately, achieving a balance with fiber intake is possible with careful consideration and planning, leading to improved gut health and stability.
Conclusion: A Holistic Approach
In conclusion, addressing SIBO through dietary adjustments involves a blend of elimination and mindful consumption. It’s essential to approach gut health holistically, considering various elements like individual tolerance, hydration, fiber intake, and even emotional wellbeing. Regularly evaluating dietary choices helps in creating a sustainable plan that can support recovery and symptom control. Collaborating with healthcare professionals ensures that diet remains balanced and tailored appropriately. Life with SIBO can be challenging, yet understanding the impact of these changes can greatly improve the quality of life. Adopting a combination of these best practices promotes not only gut health but also overall health. Having support systems, including dietitians and medical professionals, can make the journey smoother. Patients must remain proactive about tracking symptoms and adjusting their plans as necessary. Mindful eating practices across varied meal experiences offer both opportunities for pleasure and healing. With patience and persistence, managing SIBO effectively becomes possible, leading to brighter digestive health outcomes.
Each person’s experience with SIBO is unique, and while the dietary strategies discussed play a crucial role, they should be adapted to fit individual lifestyles and preferences. Finding joy in food, even within the limitations, is essential for emotional and physical wellbeing. Constantly testing new recipes and approaches can foster creativity in the kitchen, transforming the journey of recovery into an enjoyable exploration. Awareness of personal triggers allows individuals to navigate their diets while reducing symptoms. Frequent consultation with healthcare providers provides further reinforcement and encourages sustained motivation for dietary changes and symptom management. Remember, this dietary journey may not yield results overnight. Some may find certain foods tolerant while others do not, so persistence is vital. The more the individual learns about their body’s responses and unique needs, the better equipped they are to manage their condition. Ultimately, empowering oneself with knowledge about gut health leads to better choices and healthier outcomes. Through research and support networks, individuals can thrive while living with SIBO, ensuring that their diets enhance their health. Continuous exploration, learning, and adaptation are the keys to successfully navigating life with SIBO.