Emerging Research on Gut Microbiome Modulation by Various Pharmaceuticals
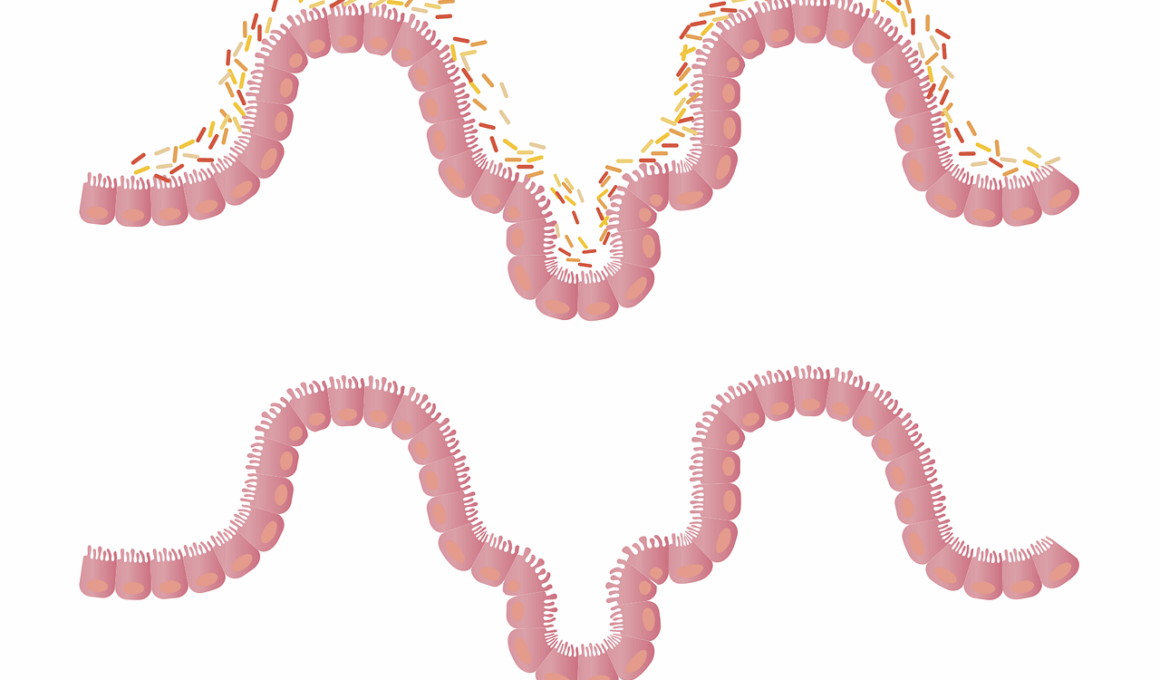
The gut microbiome plays a crucial role in human health, influencing digestion, immunity, and even mood. Recent studies indicate that pharmaceuticals can significantly impact the composition and function of the gut microbiome. Medications such as antibiotics, antacids, and probiotics are being investigated for their effects. While antibiotics can disrupt gut bacterial balance, probiotics promote beneficial bacteria growth. Understanding these interactions is essential for creating effective treatments and maintaining gut health. Furthermore, research has uncovered that the gut microbiome may mediate the effects of drugs on the body. For instance, some medications rely on gut bacteria for metabolism, thus making the microbiome’s state critical. This modulation can lead to altered drug efficacy and side effects. Continued exploration of this interface between medications and the gut microbiome could provide new perspectives on personalized medicine. Awareness of these factors is vital for healthcare providers when prescribing treatments. Considering the microbiome in medication routines can enhance patient outcomes and minimize adverse reactions. As this field of research evolves, it may yield groundbreaking implications for the development of future therapeutics.
Studies have shown that not only antibiotics but also non-antibiotic medications can affect gut microbiota. For example, long-term use of proton pump inhibitors (PPIs) has been linked to changes in the composition of gut bacteria. Emerging evidence suggests individuals using these medications might have an increased susceptibility to gastrointestinal infections. Additionally, drugs affecting dopamine pathways are associated with significant influences on gut flora. Medications like selective serotonin reuptake inhibitors (SSRIs) demonstrate how mental health medications can alter the microbiome. Increased understanding of microbiome-drug interactions is paving the way for innovative approaches to treatment. Personalized medicine that considers these interactions can lead to medications tailored to individual gut microbiota profiles. Further exploration is essential for understanding how medications can be optimized based on gut health status. The significance of the microbiome extends beyond digestion, encapsulating a holistic view of wellness. Health practitioners must remain informed about the impacts of medications on gut microbiota for informed treatment strategies. By integrating emerging research with clinical practices, healthcare can advance significantly. Building a roadmap that emphasizes the importance of the gut microbiome in pharmacology has the potential to transform multiple medical fields.
The Complexity of Gut Health
The complexity of the human gut microbiome cannot be overstated. Numerous microorganisms, including bacteria, fungi, and viruses, contribute to this dynamic ecosystem. The balance among these microbes is influenced by diet, lifestyle, and, importantly, medications. Drug interactions with gut flora create a ripple effect on health outcomes. Recent findings suggest that a rich and diverse gut microbiome can bolster drug efficacy while mitigating side effects. Understanding this complex interplay offers exciting research opportunities. Some studies indicate that certain dietary interventions combined with pharmaceuticals can optimize therapeutic outcomes. For example, prebiotics might enhance the benefits of specific medications by fostering the growth of beneficial bacteria. Conversely, certain foods can diminish drug absorption or activity. Recognizing these interactions may guide clinicians in developing better treatment plans. Additionally, the gut microbiome’s role in drug metabolism highlights the need for comprehensive research on microbiome-specific responses. Each person’s microbiome is unique, emphasizing the potential of personalized approaches in medicine. As we unveil more aspects of this relationship, we can advance our understanding of both microbiology and pharmacology, enhancing patient care significantly.
Research has shown that the impact of various medications on gut microbiota is not uniform. Some individuals experience drastic changes in their microbiome following antibiotic treatments, while others show minimal effects. This variability can stem from genetic differences, lifestyle choices, and existing microbial diversity. Such differences are essential when considering how to mitigate potential adverse effects associated with some medications. For instance, strategies aimed at restoring gut balance post-antibiotics often include probiotics or moderate dietary shifts. Employing these methods has been shown to enhance recovery of microbial populations, promoting overall gut health. Nonetheless, the timing of probiotic introduction in relation to antibiotic administration is critical for optimal benefits. Ongoing studies strive to identify which specific probiotics yield the most positive effects on different individuals, adding layers of complexity to these findings. Understanding these intricate mechanics relies on continuous research in microbiome dynamics. Researchers are now beginning to delve deeper into patient-reported outcomes and microbiome sequenced data. This promising direction will ultimately lead to improved therapeutic strategies designed for individual microbiome profiles, enhancing the overall efficacy of pharmaceuticals, and maintaining a healthy gut microbiome.
Clinical Implications of Microbiome Research
The clinical implications of recent microbiome research are profound and multifaceted. As healthcare approaches evolve, there is a growing emphasis on integrating gut microbiome analysis into clinical settings. Healthcare providers are encouraged to consider how medications influence individual microbiota and, subsequently, patients’ overall wellbeing. With a deeper understanding of microbiome interactions, practitioners can develop targeted, customized treatment plans. The introduction of microbiome-based diagnostics allows for early detection of potential adverse reactions, especially in patients on long-term medication regimens. This proactive approach can significantly enhance patient safety and therapeutic success rates. Additionally, the concept of microbiome modulation is yielding promising therapies aimed at rebalancing gut flora. These innovations have the potential to prevent antibiotic-associated disruptions or restore balance after such treatments. The rise of microbiome research signals a shift in how we perceive health and disease management. Integrating this knowledge into practical healthcare technologies will also inform public health strategies. Addressing gastrointestinal health comprehensively leads to improved outcomes across various medical conditions, emphasizing the symbiotic nature of microbiota and pharmaceuticals in our health journey.
Patients and healthcare providers alike must engage in open dialogues about the importance of gut health relative to medication use. Empowered by recent findings, patients can make informed choices regarding their medication options and support their microbiome health simultaneously. Knowledge about potential side effects stemming from medication-induced dysbiosis can foster a collaborative relationship between patients and providers. For instance, individuals on long-term antibiotics may benefit from supplementary probiotics and dietary adjustments. This informed approach empowers patients to take an active role in managing their health. Encouraging proactive discussions surrounding medications and microbiome health can enhance adherence to treatment plans and foster more positive outcomes. Additionally, sharing information on the potential to counteract negative holiday consequences reinforces the necessity of balanced gut flora to maintain overall well-being. It remains pivotal that both patients and clinicians prioritize gut health through preventative measures and continued education. Future studies can further elucidate the complex relationships between medications and the gut microbiome. By combining insights from various disciplines, we are on the frontier of more holistic healthcare approaches.
Conclusion: The Future of Gut Microbiome Research
The field of gut microbiome research offers tremendous promise for medical advancements. As researchers delve deeper, a clearer picture of how pharmaceuticals interact with the gut microbiome is emerging. Modern medicine is witnessing a paradigm shift towards personalized approaches recognizing the individuality of each patient’s microbiome. This holistic perspective is essential in addressing chronic health concerns related to gut health, which can arise from poor medication management and imbalanced microbiota. Addressing these concerns through evidence-based interventions can lead to improved drug efficacy and minimized adverse effects. Moreover, the development of microbiome-targeted therapies can revolutionize treatment strategies, amplifying the potential for tailored healthcare. Research will continue to shed light on the intricacies of gut microbiome modulation by various pharmaceuticals. Future breakthroughs will accommodate the growing interest in how medications can not only treat ailments but can also harmonize with our microbiomes. Collaborative efforts among scientists, clinicians, and patients will underpin successful implementation of this frontier research. An informed approach in the healthcare community will pave the way toward a healthier population with optimized medications that respect the microbiome.
The journey of understanding how medications impact the gut microbiome is just beginning. Growing evidence and emerging studies will illuminate the multifaceted interactions between pharmaceuticals and gut health. It is imperative to stay attuned to evolving research in this field, guide clinical practice, and promote healthy lifestyles. Recognizing the critical role of the microbiome in overall health underscores the necessity of investigating the consequences of medication on gut flora. In doing so, we can ensure a future where healthcare encourages gut health through responsible medication use. Through this lens, healthcare professionals can be more effective in mitigating adverse reactions while maximizing therapeutic outcomes. Thus, fostering improved patient experiences and satisfaction through holistic care remains the goal. So, as research continues to evolve, current paradigms of therapy must adjust accordingly. Engaging with these discoveries can catalyze a shift towards more informed decision-making in the healthcare sector. Ultimately, forging pathways that seamlessly integrate microbiome awareness into routine clinical practice will redefine health management in the years to come.