Mood Disorders and Gut Health: Emerging Research Insights
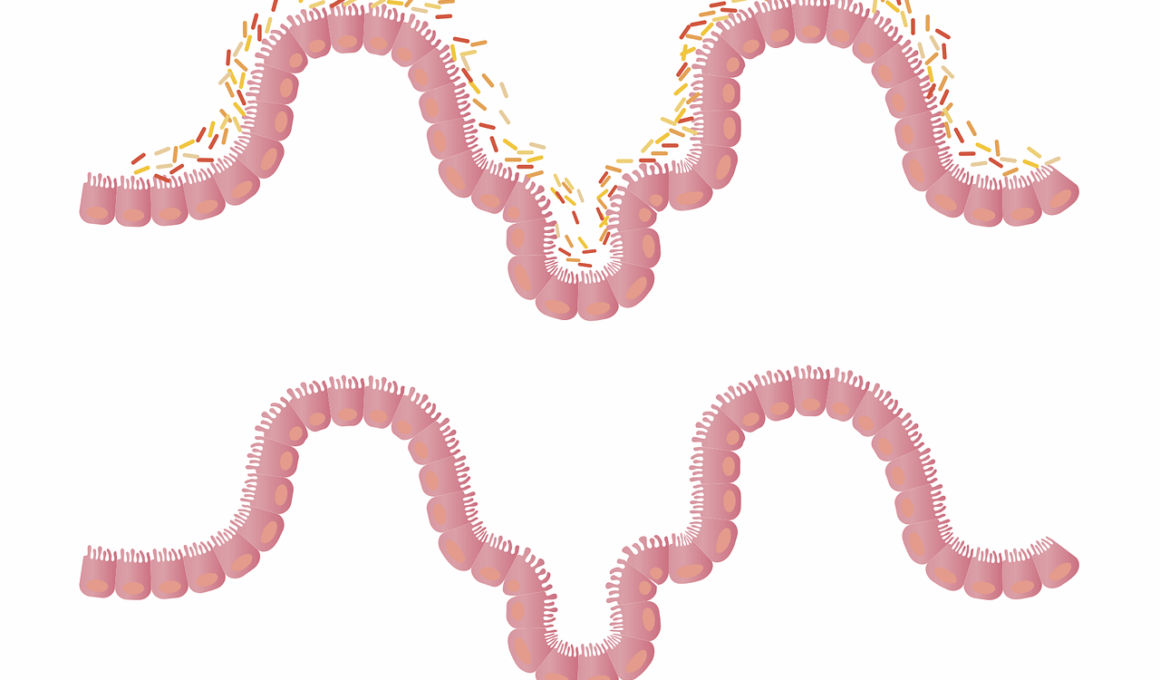
Recent studies underscore a compelling connection between our gut health and mental well-being. The gut microbiome, a complex ecosystem of bacteria, plays a crucial role in our emotional health. This interaction highlights how digestive health can profoundly impact mood disorders such as depression and anxiety. Gut bacteria can influence the production of neurotransmitters, which are vital for regulating mood. For example, approximately 90% of serotonin, a key neurotransmitter associated with happiness, is produced in the gut. Furthermore, the gut-brain axis, a bidirectional communication system, facilitates the exchange of information between the gut and the brain, affecting mental health outcomes. Research also suggests that a balanced microbiome may protect against mood disorders, while dysbiosis, an imbalance in gut bacteria, could exacerbate symptoms. Incorporating probiotics and prebiotics through diet can therefore enhance gut health and potentially alleviate mood-related symptoms. As such, there is a growing emphasis on integrating gut health strategies into treatment plans for mood disorders. Understanding this intricate relationship between gut and mind can offer new therapeutic avenues for those struggling with emotional challenges.
The Impact of Diet on Mood Disorders
The relationship between diet, gut health, and mood cannot be overstated. Certain dietary patterns are linked to the presence of specific gut bacteria, which can significantly influence mental health. A diet high in processed foods, sugars, and unhealthy fats can contribute to an unhealthy gut microbiome, potentially leading to mood disorders. Conversely, a Mediterranean diet rich in fruits, vegetables, whole grains, olive oil, and fish has been shown to support not only gut health but also mental wellbeing. Foods such as fermented products like yogurt and kimchi contain probiotics which promote a healthy microbial balance. Omega-3 fatty acids, found in fatty fish, nuts, and seeds, also possess anti-inflammatory properties that may reduce symptoms of depression. Additionally, dietary fiber plays a crucial role in promoting gut bacteria diversity, which is essential for both gut and mental health. Individuals should consider incorporating more whole, nutrient-dense foods into their diet to enhance both their gut microbiome and mood. The positive outcomes arising from such dietary changes suggest a promising area for further research in treating mood disorders through nutrition.
Emerging research continues to explore the therapeutic potential of probiotics in treating mood disorders. Probiotics, which are live microorganisms beneficial for gut health, might also improve mental health conditions like depression and anxiety. Recent studies indicate that certain strains of probiotics can influence mood-regulating processes in the brain, thereby alleviating symptoms of mood disorders. For instance, a review of clinical trials showed that individuals taking probiotics reported significant reductions in depressive symptoms compared to those on placebo treatments. This effect may stem from the modulation of the gut-brain axis, where changes in gut microbiota influence brain function and behaviour. Moreover, some researchers suggest that gut inflammation can contribute to mood disorders, and probiotics may reduce this inflammation effectively. However, while preliminary findings are encouraging, more extensive, rigorous studies are essential to validate these associations definitively. As such, individuals experiencing mood disorders may find it beneficial to consult healthcare professionals about incorporating probiotics into their treatment plans. Optimizing gut health could serve as a complementary approach toward achieving better mental health outcomes in those suffering from various mood disorders.
Your mental health is also tightly linked to various environmental factors alongside gut health. Stress, lifestyle choices, and biological predispositions all play critical roles in determining mental health status. For instance, chronic stress can lead to dysbiosis, contributing to a decline in gut health and subsequent mood disturbances. Working to manage stress through meditation, exercise, and mindfulness techniques can be integral. Exercise, in particular, has been shown to boost gut health through increased diversity and activity of gut microbiota while simultaneously promoting the release of endorphins, which positively influence mood. Furthermore, sleep quality is paramount in maintaining both gut and mental health. Poor sleep patterns can disrupt gut microbiota, which can, in turn, affect mental health negatively. Integrating balanced sleep schedules, stress management techniques, and regular physical activities might potentiate the gut-brain connection. Enhancing one’s lifestyle through these facets can lead to improved overall well-being, benefiting gut and mental health. As our understanding of these interrelations evolves, comprehensive strategies targeted at lifestyle modifications may hold the key to effective interventions for mood disorders.
The significance of mental health awareness in relation to gut health is becoming more recognized. Many individuals struggling with mood disorders may not immediately consider how gut health contributes to their symptoms. Educating patients about this connection can empower them to take an active role in their treatment. Furthermore, integrative approaches that combine traditional mental health therapies with nutritional interventions focused on gut health are gaining traction. Such integrative models may encourage adherence to treatment by addressing underlying physiological factors in mood disorders. Mental health professionals and nutritionists might work collaboratively to develop personalized dietary plans aimed at improving gut microbiota. This interdisciplinary approach could potentially enhance treatment outcomes for individuals experiencing mood disturbances. Additionally, workshops and resources promoting gut health awareness can further disseminate this knowledge to a broader audience. As research continues to explore the gut-brain connection, it is essential for healthcare providers to consider type of interventions that encompass both mental and digestive health components. Moving forward, fostering a deeper understanding of gut health’s role can ultimately lead to enhanced therapeutic strategies for mood disorders.
Taking Steps Towards Better Gut Health
Individuals seeking to improve their gut health can begin implementing dietary changes and lifestyle modifications systematically. Consuming a well-balanced diet rich in diverse foods helps lay the foundation for a healthy microbiome. Emphasizing whole, unprocessed foods, coupled with adequate hydration, supports overall digestive health. Additionally, incorporating fermented foods can introduce beneficial bacteria into the gut, enhancing microbial diversity. It’s similarly critical to avoid over-consumption of processed foods high in sugar and unhealthy fats which can negatively impact gut health. Engaging in regular physical activity can positively diversify gut bacteria associated with mood enhancement. Furthermore, as previously noted, managing stress through various techniques like meditation or yoga may have a profound impact on both gut and mental health. Adequate sleep, typically ranging from seven to nine hours, also supports gut health, thereby enhancing mood. Being proactive about implementing these changes can yield comprehensive benefits. By understanding and addressing the factors affecting gut health, individuals may foster improvements in mental health, creating a positive cycle of well-being. Taking these steps might not only improve mood but also promote overall health and resilience against future disorders.
In conclusion, the intricate links between gut health and mental well-being highlight the need for ongoing research in this dynamic field. Emerging insights into how gut microbiota influences mood disorders may help shape new therapeutic strategies. As societies acknowledge the growing epidemic of mood disorders, looking beyond conventional theories to encompass gut health could pave the way for more effective treatments. Collaborative efforts between healthcare professionals across disciplines may yield enhanced holistic treatment paradigms. Further, as public awareness of gut health’s significance increases, more individuals may recognize its role in mental well-being. This could potentially lead to greater acceptance of dietary and lifestyle interventions as vital components of mental health treatment plans. Encouraging diverse research methodologies will amplify understanding of this relationship. Concurrently, educational programs targeting mental health may proactively include discussions on gut health, ensuring individuals possess the tools needed to improve their emotional well-being. The journey toward mental wellness can be bolstered through informed decisions focused on gut health, highlighting a newly emerging paradigm in mental health care. Stronger connections between mind and gut emphasize the need for a holistic approach to mental health management, making this a crucial area for further exploration.