Fasting and Metabolic Syndrome: Strategies and Outcomes
Metabolic syndrome is a cluster of conditions characterized by increased blood pressure, excess body fat around the waist, and abnormal cholesterol levels. These factors significantly raise the risk of heart disease, diabetes, and stroke. Research indicates that fasting can serve as a potential intervention to mitigate these risks. Fasting induces beneficial metabolic changes, such as improved insulin sensitivity, reduced inflammation, and enhanced fat oxidation. Various fasting strategies exist, including intermittent fasting and time-restricted eating. They allow individuals to alternate between periods of eating and fasting, which can improve metabolic health. Benefits often include weight loss, lower blood pressure, and improved lipid profiles. However, these outcomes depend on the nature of the fasting regimen and individual health conditions. Consulting with healthcare professionals before starting any fasting protocol is crucial. It ensures the chosen approach aligns with personal health needs and circumstances. By incorporating fasting into a balanced lifestyle, individuals may effectively manage metabolic syndrome and reduce the associated health risks. This integrated approach combines diet, physical activity, and mental well-being, collectively aiming for better health outcomes.
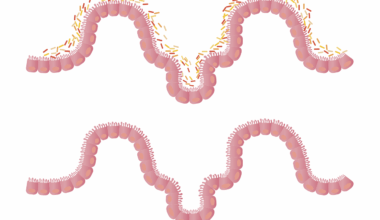
One popular method in fasting is intermittent fasting, which alternates periods of eating with periods of not eating. This practice is often characterized by methods such as the 16/8 approach, where individuals fast for 16 hours and have an 8-hour eating window. Studies suggest that intermittent fasting can lead to a significant decrease in visceral fat, particularly around the abdominal area, which is critical for individuals with metabolic syndrome. Visceral fat is closely linked to insulin resistance and cardiovascular diseases. Regular intermittent fasting may help lower blood sugar levels and improve insulin sensitivity, effectively combating the challenges of metabolic syndrome. It can also lead to weight loss, which is vital for managing overall health. Furthermore, fasting has shown potential in reducing markers of inflammation, such as C-reactive protein. This reduction contributes to a lower risk of heart disease and other related complications. While the benefits are promising, consistency and adherence to the fasting schedule play pivotal roles in achieving lasting results. Individuals are encouraged to find a fasting method that fits seamlessly into their lifestyles for long-term success in managing health outcomes.
Time-restricted eating is another effective fasting strategy that focuses on the timing of meals. This approach typically restricts eating to a specific time frame each day, often spanning 6 to 10 hours. For example, one might eat between 12 PM and 8 PM, fasting for the remaining 16 to 14 hours. Research indicates that time-restricted eating can promote weight loss, improve glucose metabolism, and reduce blood pressure. This improved metabolic profile is particularly beneficial for individuals dealing with metabolic syndrome. By limiting caloric intake to a specified window, individuals may experience a natural reduction in calorie consumption without the need to count calories. Additionally, time-restricted eating aligns with the circadian rhythm, which may enhance metabolic efficiency. Early studies have suggested a correlation between time-restricted eating and reduced fat mass, increased lean body mass, and overall improved metabolic markers. Importantly, individuals should prioritize nutritious foods during eating periods to maximize health benefits. Overall, time-restricted eating can be a practical and sustainable method for managing metabolic syndrome and improving overall wellness.
Potential Risks and Considerations
While fasting presents numerous benefits, there are potential risks and considerations that should not be overlooked. Individuals with certain medical conditions, such as diabetes or eating disorders, may face complications when fasting. For those on medications for diabetes, fasting can lead to dangerously low blood sugar levels, necessitating close medical supervision. Additionally, individuals who experience significant calorie deficits during fasting might encounter fatigue, irritability, and difficulty concentrating. Prioritizing hydration during fasting periods is essential. Fasting may also result in nutrient deficiencies if not planned carefully. Ensuring adequate intake of essential nutrients during eating windows is critical for overall health. Setting realistic expectations is equally important; while methods may yield significant health improvements for some, results can vary widely among individuals. Therefore, tailored fasting plans designed with professional guidance ensure safety and effectiveness. Individuals should also monitor their bodies’ responses throughout the fasting process. Listening to one’s body is integral to establishing a sustainable fasting routine. Ultimately, understanding the benefits and risks helps individuals navigate their fasting journey effectively.
Combining fasting with physical activity can further enhance health outcomes, especially for those managing metabolic syndrome. Regular exercise complements the benefits of fasting by improving cardiovascular fitness and aiding weight management. Physical activity can boost metabolism and support the body’s adaptation to fasting periods. Additionally, engaging in consistent exercise may heighten insulin sensitivity, working synergistically with fasting to mitigate the effects of metabolic syndrome. Various forms of exercise, including aerobic and strength training, can significantly contribute to these improvements. Including at least 150 minutes of moderate aerobic activity weekly is recommended to achieve optimal health benefits. Exercise also supports mental well-being, which may be influenced during fasting periods. Adopting a holistic lifestyle approach incorporating diet, exercise, and mental health practices is essential for effective management. Furthermore, sharing experiences with support groups or health coaches can provide motivation and accountability. Individuals can craft personalized plans that seamlessly integrate fasting and exercise, allowing for sustainable lifestyle changes. By fostering a balanced approach, individuals may achieve lasting improvements in metabolic syndrome outcomes.
Monitoring Progress and Staying Motivated
Monitoring progress during fasting is vital for maintaining motivation and achieving desired health outcomes. Individuals should track various metrics, including weight, body measurements, and metabolic markers, to assess their progress. Cleansing diets during fasting periods often yield initial weight loss, driven by water loss and glycogen depletion. Being aware of these initial changes can provide insight into individual body responses. Furthermore, noting changes in energy levels, mood, and overall well-being is crucial. These metrics help individuals understand the broader effects of fasting beyond just weight loss. Setting short-term and long-term goals fosters commitment to the fasting process. Celebrating small milestones reinforces motivation and boosts morale. Engage with online communities or social media platforms to share experiences, challenges, and successes. These interactions cultivate a supportive environment for those embarking on similar journeys. Documenting progress in journals or apps can also yield valuable reflections and insights. Ultimately, the combination of self-monitoring, social support, and goal-setting plays a key role in sustaining motivation throughout the fasting experience.
In conclusion, fasting shows significant potential for managing metabolic syndrome, providing a multitude of health benefits when practiced effectively and safely. By exploring various fasting strategies such as intermittent fasting and time-restricted eating, individuals can improve metabolic health outcomes. Understanding the importance of consulting healthcare professionals ensures responsible implementation, particularly for those with underlying health conditions. Integrating physical activity into fasting regimens enhances results, while attention to individual body responses helps in tailoring practices. Moreover, setting goals and monitoring progress fosters accountability. Individuals should strive for a balanced approach to achieve lasting improvements in health. Ultimately, fasting can empower individuals to take charge of their metabolic health, reduce the risks associated with metabolic syndrome, and foster a healthier lifestyle continuing beyond fasting. As research into the benefits and methods of fasting expands, it becomes increasingly clear that with the right strategies and support, fasting can be a formidable ally in the journey toward improved health and well-being. Embracing these practices might unlock a sustainable pathway to not just manage but thrive amid the challenges posed by metabolic syndrome.
- References
- Cureus Journal on Metabolic Syndrome
- National Institutes of Health
Fasting and its role in metabolic syndrome have become subjects of much ongoing research. Multiple studies underscore its importance for cardiovascular health, insulin resistance, and weight management. Emerging findings contribute valuable insights into how fasting can be integrated into personal health strategies. Remaining informed and engaged with the latest research in this area can guide individuals on their fasting journey. Knowledge empowers better decision-making for health interventions. By acknowledging the core principles governing fasting and metabolic syndrome, combined with credible sources, individuals may more effectively navigate their healthcare choices. Integrating the latest findings into daily practices fosters a deeper understanding. Healthy collaborations with healthcare professionals aid in creating personalized fasting plans tailored to individual needs. As exploration continues, fasting holds promise as a legitimate therapeutic tool in addressing metabolic health challenges.