Diverticulitis and Its Relationship to Gut Microbiome
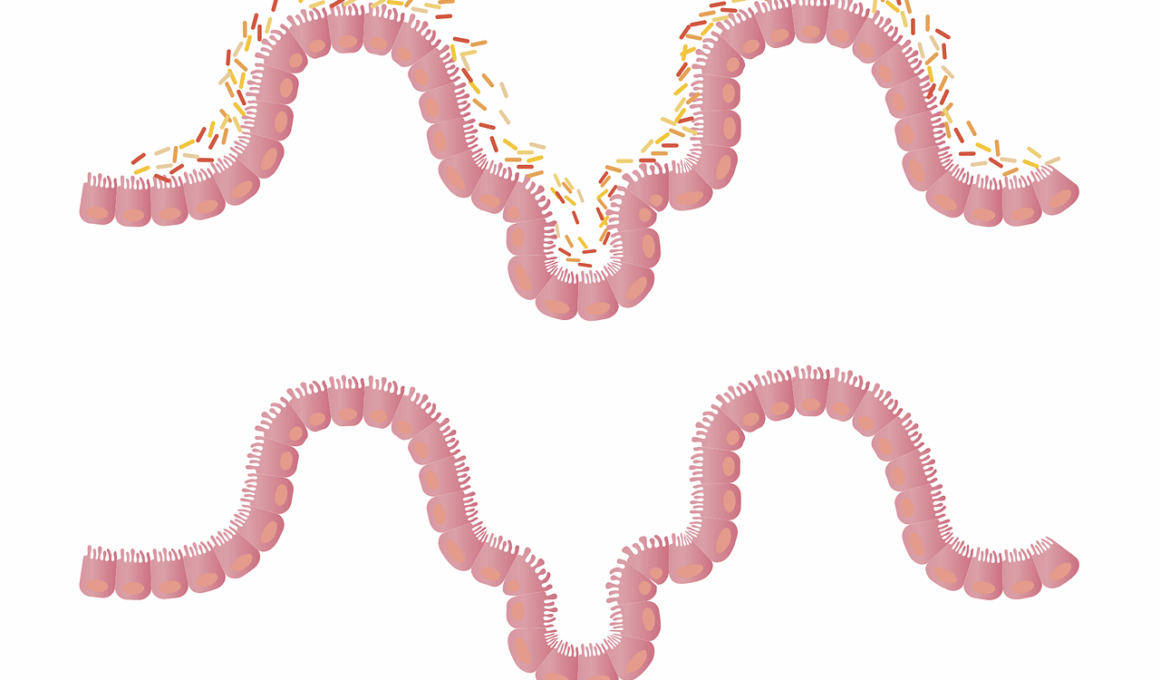
Diverticulitis is an inflammatory condition affecting the digestive tract, primarily seen in individuals aged over 40. This health issue arises when diverticula, small pouches formed in the colon lining, become inflamed or infected. The relationship between diverticulitis and the gut microbiome has gained significant attention in recent years. A healthy gut microbiome usually supports proper digestion, but disruptions in microbiota may lead to complications. Some studies suggest that an imbalance in gut bacteria can contribute to the development of diverticulitis. This condition often presents with symptoms such as abdominal pain, fever, and changes in bowel habits, emphasizing the need for comprehensive management strategies. Treatment often includes dietary modifications, antibiotics, and in severe cases, surgery. Patients with diverticulitis may also benefit from probiotics, which are known to positively influence gut health by restoring microbial balance. Understanding the role of gut microbiome in diverticulitis can lead to innovative treatment options and preventive measures, improving the overall health of affected individuals. Research continues to explore the influence of lifestyle factors on microbiome diversity and how they impact conditions like diverticulitis.
Emerging research highlights the importance of a balanced gut microbiome in preventing diverticulitis. Unhealthy dietary habits, including high-fat and low-fiber diets, contribute to imbalances in gut microbiota. Introducing a fiber-rich diet can facilitate better digestion while promoting the growth of beneficial bacteria. Fruits, vegetables, whole grains, and legumes are excellent sources of fiber that improve gut health. Additionally, a low intake of dietary fiber can lead to increased intraluminal pressure, a contributing factor to diverticular formation. Including foods with prebiotics and probiotics can further enhance gut microbiome balance. Studies indicate that consuming fermented foods such as yogurt and kefir may lower the risk of diverticulitis flare-ups. Likewise, prebiotic foods like garlic, onions, and bananas feed good bacteria, supporting microbiome diversity. The idea is to create an environment where healthy bacteria thrive, particularly in the lower gastrointestinal tract. Ongoing investigations focus on how specific strains of bacteria can moderate inflammation associated with diverticulitis. This knowledge can provide better dietary and therapeutic guidelines for individuals predisposed to this condition.
Dietary Interventions for Diverticulitis Management
Dietary interventions are essential for managing diverticulitis and restoring gut microbiome balance. Healthcare providers often recommend a gradual introduction of high-fiber foods after an acute diverticulitis attack. This approach ensures that the digestive system has adequate time to heal before facing more complex foods. Gradually reintroducing fiber helps prevent recurrence while encouraging microbial diversity. Patients can choose between soluble and insoluble fibers, which each play a distinct role. Soluble fiber can improve gut motility and reduce inflammation, whereas insoluble fiber aids in stool consistency and movement. Remember that hydration is key when increasing fiber intake, preventing potential complications, such as constipation. In addition to fiber, incorporating antioxidants found in fruits and vegetables can help reduce inflammation in the gut. Furthermore, avoiding processed foods, excess sugar, and unhealthy fats can significantly affect microbiome health. Staying mindful of food choices helps individuals manage diverticulitis more effectively, ultimately leading to a better quality of life. Individual dietary recommendations vary, showcasing the need for personalized approaches to treat gut disorders like diverticulitis.
In addition to diet, lifestyle factors such as stress management and regular exercise are equally important for maintaining a healthy gut microbiome. Stress can adversely affect gut permeability and microbial balance. High levels of stress hormones can influence digestive function, leading to increased inflammation. Techniques such as yoga, meditation, and mindfulness can play a significant role in reducing stress and promoting gut health. Regular physical activity has also been shown to positively impact gut microbiota. Exercise can enhance gut transit time and improve overall digestive function. Building a routine that incorporates both physical activity and relaxation techniques helps maintain a balanced microbiome. Furthermore, avoiding smoking and limiting alcohol consumption can protect gut health. These lifestyle changes complement dietary interventions and form a comprehensive approach to managing and preventing diverticulitis. The integration of physical and mental wellness practices can significantly enhance the effectiveness of dietary modifications. As ongoing research continues to uncover connections between gut health, microbiome composition, and lifestyle factors, it is essential to adopt holistic strategies to prevent and manage diverticulitis.
Probiotics and Their Role in Gut Health
Probiotics are live microorganisms that can provide various health benefits when consumed in adequate amounts. These beneficial bacteria contribute to the restoration of gut microbiome balance, particularly for individuals prone to diverticulitis. Probiotics may help decrease inflammatory responses in the gut, alleviating the symptoms associated with diverticulitis. Fermented foods such as yogurt, sauerkraut, and kimchi serve as excellent natural sources of probiotics. Several studies have indicated that specific strains, such as Lactobacillus and Bifidobacterium, can be beneficial in reducing symptoms and the duration of diverticulitis flare-ups. Additionally, commercial probiotic supplements are available, but consultation with a healthcare professional is essential to choose the right strain and dosage. Knowledge about the appropriate delivery and timing of probiotics is crucial for maximizing their benefits. Furthermore, ongoing studies aim to unravel the complex interactions between probiotics and the immune system in the context of diverticulitis. Ultimately, the inclusion of probiotics as part of a comprehensive treatment strategy may improve patient outcomes, allowing them to manage the condition effectively.
It is vital to recognize the connection between diverticulitis, gut microbiome, and the overall impact on health. A well-balanced gut microbiome plays a crucial role in maintaining gut immunity, preventing unnecessary inflammation, and aiding digestion. Recurrent diverticulitis can lead to chronic complications, including abscess formation and fistulas that necessitate surgical interventions. Consistent engagement with healthcare professionals enables individuals to assess their condition and adapt treatment strategies accordingly. Routine monitoring of symptoms alongside dietary and lifestyle modifications provides comprehensive care. Educational initiatives can empower individuals to understand their gut health, which emphasizes the significance of microbiome-friendly choices. Likewise, further research is essential to explore how various dietary components, medications, and probiotics can synergistically influence gut health and diverticulitis management. The quest for solutions encourages patient involvement in their treatment plans, fostering a holistic understanding of their condition. By embracing proactive steps towards gut health, individuals can greatly enhance their quality of life, ultimately minimizing the risk of diverticulitis recurrence. Health professionals, researchers, and patients must work collaboratively to keep pushing the frontiers of knowledge regarding diverticulitis.
Conclusion and Future Directions
In conclusion, diverticulitis poses significant challenges for affected individuals, but understanding its relationship with the gut microbiome highlights potential pathways for improvement. By prioritizing a healthy diet, managing stress, and considering probiotics as part of therapeutic regimens, individuals may mitigate the impact of this disorder. The continual evolution of research provides insights into novel strategies for managing diverticulitis and fostering a better quality of life for patients. Personalized approaches, guided by healthcare professionals, can lead to effective management plans tailored to individual needs. As awareness of gut microbiome significance grows, further studies are critical for uncovering the interactions between dietary components and microbiota in preventing diverticulitis. More robust clinical trials can shed light on optimal probiotic formulations and their direct effectiveness in treating this condition. Additionally, public health education can bolster understanding of how lifestyle modifications can correlate with a reduced risk of diverticulitis. Through ongoing collaboration, there is substantial potential for evolving frameworks that promote healthier gut microbiomes and contribute significantly to diverticulitis management strategies.
While diverticulitis continues to be a prevalent concern for many, the collaborative efforts between researchers and healthcare professionals can lead to innovative solutions. They help illuminate the path forward for individuals battling diverticulitis while promoting overall gut health. Moreover, perspectives on integrating gut health principles into mainstream healthcare systems can improve patient education and accessibility to tools necessary for informed decisions. As we navigate the complexities of this condition, the importance of addressing gut microbiome health remains clear. Embracing this knowledge can convince more people to adopt healthier lifestyles, fostering positive changes that can directly affect diverticulitis outcomes. By remaining focused on gut health, medical communities can enhance existing therapeutic options, leading to a more holistic approach for patient care. This journey is not solely about treating diverticulitis, but rather about empowering individuals and encouraging them to prioritize their digestive health. As research progresses, the hope is to develop more effective approaches that complement traditional treatments for diverticulitis, significantly improving the lives of those affected.