How Antibiotics Affect Gut Microbiome and Subsequently Bone Mass
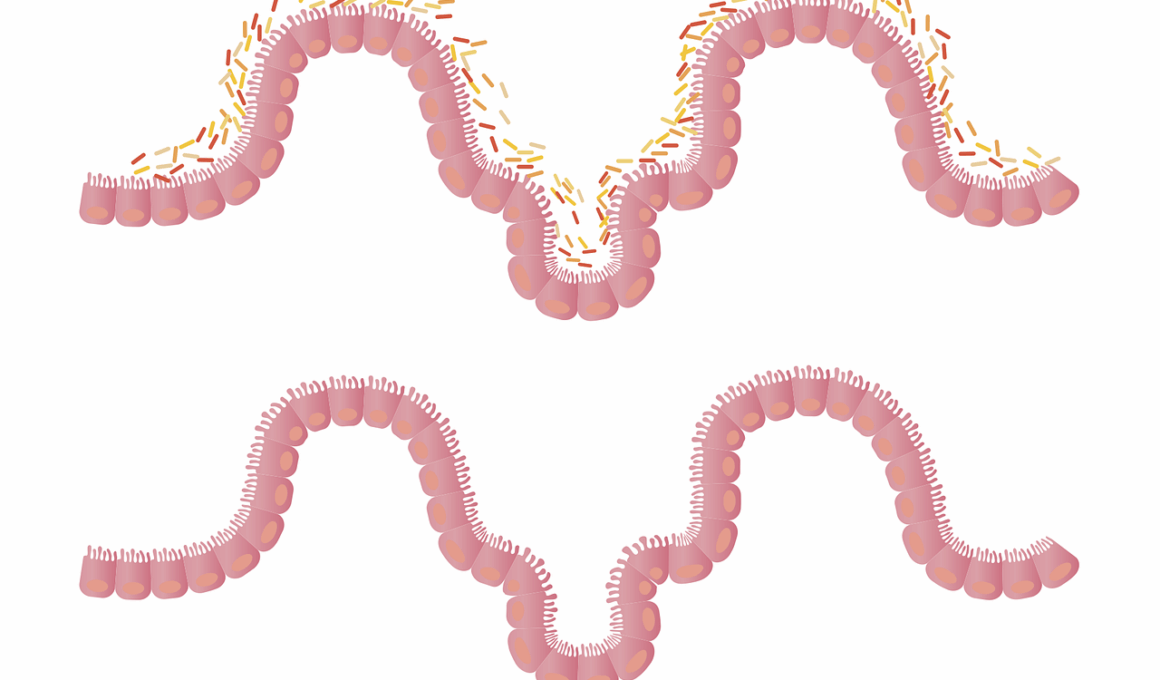
The gut microbiome is an intricate community of microorganisms residing in our intestines, playing a critical role in overall health. Research indicates that antibiotics can drastically disrupt the delicate balance of these microbial populations. Disruption occurs due to the broad-spectrum nature of many antibiotics, which can indiscriminately kill both harmful and beneficial bacteria. Consequently, this results in a diminished diversity that is crucial for a healthy gut microbiome. Various studies have linked reduced gut diversity to both metabolic disorders and bone health issues. Those with a diverse array of gut microbes tend to maintain better bone density and structure. Therefore, understanding how antibiotics pertain to this issue may illuminate further health concerns. The impact of antibiotics on gut microbiota extends beyond just immediate symptoms; it can influence long-term health outcomes, including skeletal success. Hence, maintaining a balanced microbiome is essential, particularly after antibiotic treatment. Restoration efforts, including dietary modifications and probiotics, have shown promise in rebuilding gut flora, but further investigation remains imperative.
One of the key areas of interest is the relationship between gut microbiome composition and bone health. Recent research has revealed that the gut microbiome appears to influence calcium absorption, which is pivotal for maintaining bone mass. Among the various microbial populations, specific strains can enhance the bioavailability of calcium, thus supporting bone mineralization. Conversely, the depletion of these beneficial microbes due to antibiotic use can consequently lead to decreased calcium absorption. This effect can result in a gradual decline in bone density, predisposing individuals to fractures and osteoporosis over time. Studies have demonstrated that individuals with greater microbial diversity tend to have a lower incidence of bone density loss compared to those with fewer beneficial microbes. A diverse gut microbiome functions as a protective factor, enhancing the regulation of immune responses, which also contributes to bone health. Moreover, emerging evidence suggests that specific metabolites produced by gut microbes have direct effects on bone-forming cells, indicating that microbiome modifications may have therapeutic potential in mitigating bone loss.
Impact of Antibiotics on Gut Bacteria Diversity
The impact of antibiotics on gut bacteria diversity is profound and long-lasting. Antibiotics can cause substantial reductions in microbial diversity, adversely affecting the helpful bacteria that support our bodily functions. The gut microbiota consists of trillions of microorganisms, which collaborate to maintain metabolic and immune homeostasis. Following antibiotic therapy, studies show that a significant portion of these beneficial microbes does not return to baseline levels. The residual effect can result in an imbalance, contributing to dysbiosis, an altered gut microbiome scenario that can lead to gastrointestinal issues, inflammatory diseases, and obesity. Moreover, this imbalance may also mediate adverse effects on bone health, linking antibiotic use to an increased risk of osteoporosis. Observational research emphasizes that older adults who frequently consume antibiotics are at heightened risk for skeletal-related events. Insights are beginning to emerge, proposing that strategies aimed at restoring gut microbiome composition could serve as potential interventions for bone health preservation in antibiotic users.
Probiotics have gained attention as a potential solution for restoring gut health following antibiotics. They are live microbes that, when administered in adequate amounts, confer a health benefit to the host. Various strains of probiotics can aid in repopulating the gut with beneficial bacteria, thus potentially mitigating the negative effects of antibiotic-induced dysbiosis. Probiotics are available in several forms, including supplements and fermented foods like yogurt, sauerkraut, and kefir. Research has indicated that certain probiotic strains may contribute positively to bone health by improving calcium absorption and supporting bone repair processes. Furthermore, combining probiotics with prebiotics—compounds that provide food for beneficial bacteria—can enhance gut flora restoration, creating a synergistic effect on both gut and bone health. Robust studies have also suggested that individuals who consume probiotics post-antibiotic treatment experience fewer gut-related complications and improved bone density markers. This suggests a compelling rationale for incorporating probiotics into recovery plans after antibiotic therapies, potentially presenting an avenue for preventing bone loss.
Dietary Influence on Gut Microbiome
Diet plays a critical role in shaping gut microbiome composition and subsequently bone health. A diet rich in fiber, fruits, vegetables, and whole grains fosters a healthier and more diverse gut microbiome, promoting beneficial bacteria proliferation. These dietary components typically provide prebiotic fibers, which nourish beneficial microbes and enhance microbial diversity. Furthermore, certain vitamins and minerals found in these foods also support bone mineralization. Conversely, diets high in processed sugars and unhealthy fats often correlate with diminished gut diversity and increased inflammatory responses, adversely affecting bone density. Consequently, individuals, particularly those on antibiotics, may benefit from implementing dietary changes that support gut health, ensuring adequate nutrient intake for optimal bone health. Scientific evidence underscores the interaction between dietary patterns and gut microbiome health, indicating that nutrition should be a vital focus in maintaining skeletal integrity. Developing a diet tailored to support gut health may mitigate the risk of bone-related issues, particularly in populations with a history of antibiotic use. Thus, a comprehensive approach combining diet and probiotics presents an opportunity for improved health outcomes.
Further investigation is warranted into the mechanistic pathways linking the gut microbiome and bone health. Understanding specific bacteria that contribute to bone health can unveil novel treatment strategies for osteoporosis and related conditions caused by antibiotics. Researchers are actively exploring therapeutic targets, including metabolites that gut bacteria produce, which may influence bone-forming cells directly. Furthermore, the immune-modulating properties of gut microbiota might shed light on inflammatory mechanisms known to impact bone resorption. The interplay between gut bacteria, host immune function, and skeleton integrity is an exciting area of investigation. Continued research will ideally result in personalized probiotic therapies, which restore gut balance while enhancing bone mass. Collaborations between microbiologists and osteologists may pave the way for breakthroughs in treating osteopenic and osteoporotic individuals. Each research finding provides further clarity on how maintaining a healthy gut microbiome can bolster bone health, inspiring healthcare professionals to advocate for microbiome-aware treatment regimens. This synergy between gut health and orthopedic health emphasizes a comprehensive view of holistic medicine.
In conclusion, the relationship between antibiotics, gut microbiome, and bone health is complex and bidirectional. With the growing use of antibiotics, especially in modern medicine, there’s an increasing need to understand their long-term implications on health. Patients should be informed about these effects and be encouraged to discuss strategies to support microbiome recovery post-treatment. Proactive measures, such as dietary changes and probiotic supplementation, can facilitate better gut health and, by extension, improved bone density. It’s essential for medical professionals to consider the microbial ecology in treatment protocols, especially for populations vulnerable to bone loss, like the elderly. Advocating for strategies that limit unnecessary antibiotic prescriptions while promoting gut health recovery could redefine how we approach bone health in patients. Moreover, public health campaigns might aim to raise awareness of the effects of antibiotics beyond just gut health, extending to overall well-being and skeletal health. Overall, by cultivating a comprehensive understanding of gut microbiota’s role in health, individuals can make informed choices, ultimately enhancing their health and quality of life.
Further efforts to understand the dynamics of gut microbiomes can help in predicting health outcomes accurately. Research is ongoing to identify biomarkers that may signal an unhealthy microbiome or potential bone-related issues triggered by antibiotic usage. Predictive models based on gut microbiota composition could provide clinical insights, guiding treatment strategies for at-risk individuals. Personalized medicine approaches could revolutionize how clinicians treat patients, particularly those with significant antibiotic histories. Observing changes in microbiome diversity could serve as an early indicator of impending bone health issues. Such advancements promote a proactive stance towards preserving skeletal integrity through dietary and microbial interventions. Dietary assessments may evolve to incorporate microbiome testing, thus optimizing nutritional support tailored to gut health. By integrating these practices within clinical settings, the looming negative impact of antibiotics on bone health may be mitigated. Furthermore, through collaboration between nutritionists, microbiologists, and medical practitioners, a more synergistic approach to preserving health can emerge. Ultimately, a multidisciplinary approach will allow the elucidation of underlying mechanisms and, in turn, the development of interventions aimed at strengthening both gut microbiomes and bone health.