Can Fasting Help Prevent Infections? Exploring the Evidence
Fasting has recently gained popularity not only as a means of weight management but also for its potential health benefits, particularly concerning the immune system. Research indicates that fasting can positively influence immune functionality and response to infections. The process can activate a state of autophagy, where cells remove damaged components, contributing to better resilience against diseases. Enhanced autophagy can nourish immune cells, allowing them to focus on combating infections, thus improving the overall immune response. Nevertheless, the connection between fasting and immunity is complex, with many factors coming into play. Short-term fasting may create cellular stress, which, in a positive light, can help the body prepare itself to fight infections. Regular fasting schedules might also promote metabolic flexibility, a crucial aspect of immune health. However, overextending fasting periods can lead to negative side effects, including nutrient deficiency and weakened immunity. Therefore, it is essential to approach fasting with caution, especially for vulnerable populations. Future studies need to address these intricacies to provide clearer dietary guidelines regarding fasting and its impact on the immune system.
Immune System Modulation Through Fasting
The immune system is the body’s defense mechanism, tasked with identifying and eliminating pathogens. Fasting has the potential to modulate this system in multiple beneficial ways. During fasting, certain immune cells, including lymphocytes and macrophages, can regenerate more efficiently, strengthening the immune response. Additionally, fasting may help reduce inflammation in the body, a contributor to numerous chronic diseases and infections. Lowering inflammation prepares the immune system to respond more effectively to new pathogens. Studies indicate that periodic fasting can lead to increased levels of key protective proteins such as cytokines, which play vital roles in orchestrating immune responses. Furthermore, many people report improved cognitive function during fasting periods, suggesting a stronger mind-body connection. It can be argued that a healthier mind results in better choices for overall health, including nutrition and immune support. However, moderation is crucial since excessive fasting can lead to stress and hormonal imbalances. Striking a balance is critical for achieving the desired immune benefits, highlighting fasting’s potential while recognizing its limits.
Another aspect to consider is the potential role of fasting in reducing oxidative stress, a significant factor contributing to immune dysfunction. Short-term fasting can lead to decreased levels of reactive oxygen species (ROS), which, when elevated, can harm immune cells. This decrease is crucial for immunity because oxidative stress impairs the function of immune responses, making the body more susceptible to infections. The antioxidant response may be enhanced during fasting, allowing the body to rid itself of excess oxidants and rejuvenate immune system operations. As a result, a derivation from oxidative stress may lead to improved health outcomes, particularly concerning infectious diseases. The synergy between fasting and antioxidants shows promise for holistic health approaches. However, research remains in the early stages, and while current evidence points to potential benefits, more large-scale studies must be conducted. Understanding the mechanisms by which fasting affects oxidative stress will contribute significantly to nutritional advice related to immune health. Adequate dietary choices during non-fasting periods are just as essential for maintaining a robust immune response.
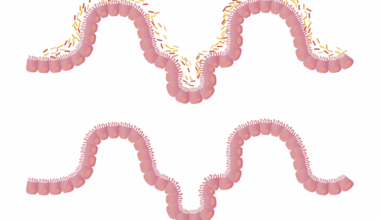
Fasting can also help enhance the gut microbiome, crucial for immune health. The gut is home to trillions of microorganisms that play a central role in regulating the immune system. A diverse microbiome can bolster defenses against infections, and fasting may help restore balanced gut flora, which has been shown to improve immunity. Research suggests that fasting positively affects gut permeability and enhances the growth of beneficial bacteria. Moreover, a healthier gut microbiome is associated with reduced inflammatory responses linked to various diseases. The interplay between fasting and gut health illustrates how interconnected bodily systems are; improving one system can yield positive effects on others. However, individuals should still prioritize nutrition during eating windows to ensure a rich intake of prebiotics and probiotics. The potential of fasting to modulate gut flora opens new avenues for research exploring potential therapeutic effects on immune problems. Ultimately, fostering a well-functioning gut through fasting might enhance overall immunity, reducing the occurrence of infections and diseases.
Potential Risks of Fasting on Immune Function
While fasting holds promise for enhancing immune responses, it comes with certain risks, particularly if done improperly. Extended periods of fasting may lead to nutritional deficiencies that can compromise immune function. Essential vitamins and minerals are crucial for maintaining a strong immune response; their absence can leave the body unable to fend off infections effectively. Furthermore, fasting may not suit everyone, especially individuals with existing health conditions, such as diabetes, where blood sugar management is vital. Stress induced by excessive fasting can also impact hormonal levels, leading to adverse immune effects. Individuals should consult healthcare professionals prior to starting extended fasting regimens. Monitoring one’s health during fasting periods is equally vital, as the balance between gaining benefits and facing drawbacks must be maintained. Educating oneself on appropriate fasting schedules and nutritional choices during eating windows can mitigate risks. The dialogue surrounding fasting needs to evolve, emphasizing that while potential benefits exist, they must be weighed carefully against the realities of individual health and lifestyle.
To summarize the potential benefits and risks of fasting concerning the immune system, it’s essential to advocate for a tailored approach. Not all fasting methods yield the same results, and personalized strategies based on individual health status could optimize outcomes. Research shows that intermittent fasting tends to benefit most average individuals by allowing cellular regeneration cycles without excessive nutrient depletion. Adapting methods according to lifestyle, preferences, and health conditions can maximize gains from fasting while minimizing risks. Dietary diversity during non-fasting periods significantly contributes to restoring nutrients necessary for immune health. The synergy between nutrition and fasting can serve as a cornerstone of preventive health strategies against infections. Recognizing each person’s unique body responses to fasting will lead to more targeted guidelines in the future. Emphasizing balance, mindfulness, and moderation during fasting periods can pave the way for maintaining a strong immune system. Continued exploration into how different fasting patterns interact with individual biochemistry is necessary for advancing nutritional science and health.
Conclusion and Future Research Directions
In conclusion, the role of fasting in relation to immune health presents an intriguing avenue for future research. Current studies suggest potential benefits, yet more extensive and rigorous trials are required to determine optimal fasting practices for promoting immunity. Understanding individual variations in response to fasting can inform more effective recommendations, making nutritional advice more precise and personalized. Researchers might focus on specific pathways linking fasting and immune modulation to create scientifically-backed dietary guidelines. Future investigations should also analyze long-term effects of fasting on overall health and specific populations, especially those more susceptible to infectious diseases. Incorporating biochemical analyses of immune responses during fasting could deepen knowledge on how fasting protects against infections. Advances in nutrition science approach this subject with curiosity. A holistic viewpoint considering lifestyle, stress, exercise, and psychological health alongside fasting’s advantages may yield comprehensive insights. As research progresses, society can glean beneficial information on the health of our immune systems, allowing for informed decisions on dietary practices, especially related to fasting.
Ultimately, as fasting continues to draw attention as an influential health practice, its implications for immune function illustrate the interconnectedness of body systems. Fasting isn’t merely a form of calorie restriction but a dynamic way to engage our bodies’ fundamental processes. By adopting respectful and informed fasting practices, individuals may harness its potential benefits while recognizing the present limitations involved. Understanding these complexities will guide future health practices and nutritional recommendations centered on enhancing immunity and overall wellness. Education around fasting should celebrate its capabilities while cautiously approaching its risks, promoting informed choices for individuals’ different contexts. The narrative surrounding fasting should evolve alongside the research, offering transparent insights into its efficiency and viability. With proper guidance, fasting may emerge as an empowering strategy for enhancing immune health, paving the way to a healthier and more resilient public. As ongoing studies shed light on these relationships, new avenues for self-care and nutrition will unfold, ensuring fast-paced lifestyles don’t compromise our health. The increasing understanding will encourage holistic health approaches, ensuring people can thrive amid challenges.