Sleep Disruption as a Marker for Inflammatory Diseases
Understanding the relationship between sleep and inflammation is crucial to grasping how sleep disruption can affect overall health. Research highlights that poor sleep can increase inflammatory markers within the body. When inflammation occurs, it often leads to chronic diseases such as heart disease, diabetes, and autoimmune disorders. The impact of inadequate sleep has gained attention from scientists exploring its role in inflammation. Inflammatory cytokines are released during poor sleep patterns and can heighten the risk of these conditions. Additionally, chronic inflammation can lead to even more profound sleep issues, creating a vicious cycle. Therefore, addressing sleep quality must be a priority for anyone facing health challenges. Researchers have observed how sleep deprivation can elevate levels of C-reactive protein and interleukin-6, two markers linked to inflammation. These findings suggest that enhancing sleep might reduce inflammation, consequently lowering disease risk. Individuals suffering from sleep disorders may benefit significantly from monitoring their sleep patterns and seeking supportive therapies. Proper sleep hygiene practices can be introduced as part of a holistic approach to managing inflammation.
The connection between sleep patterns and inflammation also sheds light on potential interventions. Sleep quality can undergo significant improvement through lifestyle modifications. Regular sleep schedules, a comfortable sleep environment, and reducing stimulants before bedtime can lead to better rest. Furthermore, incorporating relaxation techniques can contribute to deeper sleep and fewer awakenings, thus promoting healing. Engaging in regular physical activity may also enhance sleep quality while reducing inflammation. Physical exercise has a profound effect on overall health and can help manage weight, another key factor in inflammation levels. A balanced diet, rich in anti-inflammatory foods, might even improve sleep quality. For instance, omega-3 fatty acids found in fish can reduce markers of inflammation. It’s important for individuals to understand sleep’s role in health and take proactive measures. Experts suggest that following a regular routine that includes winding down can aid in preparing the body for restful sleep. Incorporating mindfulness practices such as meditation can also improve sleep quality. By creating an environment that fosters relaxation, individuals may experience lower inflammatory responses, enhancing their health over time.
Chronic sleep deprivation is increasingly recognized as a risk factor for various inflammatory diseases. Studies have shown that insufficient sleep disrupts the body’s natural regulatory systems. This disruption results in heightened inflammation and potential disease development. Sleep’s restorative functions are not merely beneficial; they are essential for maintaining a healthy immune system. The body’s inflammatory response relies heavily on proper sleep architecture, including the stages of deep sleep. Deep sleep facilitates recovery and cellular repair, while inadequate amounts can lead to increased susceptibility to infections. Furthermore, repeated sleep disruption may create a state of chronic inflammation that can affect longevity. Sociocultural factors often contribute to sleep deprivation, such as work demands, stress, and lifestyle choices. Identifying these issues is crucial in tackling the bigger picture of inflammation management. It’s essential for individuals to prioritize their sleep for long-term health benefits. Health professionals encourage integrating sleep assessments in routine medical check-ups to better understand how these factors correlate. Recognizing patterns early can lead to effective interventions that prioritize proper sleep as an integral aspect of health routines.
The Mechanism Behind Sleep and Inflammation
Recent advances in research have elucidated the mechanisms linking sleep and inflammation. During sleep, especially during the rapid eye movement (REM) phase, cytokines are released that contribute to the immune system’s regulation. Insufficient sleep can hinder this process, resulting in a pro-inflammatory state. Disruptions in sleep quality can alter cortisol levels, which play a significant role in regulating inflammation. Cortisol, often referred to as the stress hormone, is vital for maintaining homeostasis in the body. Chronic dysregulation from poor sleep can exacerbate inflammatory markers and increase the risk of chronic diseases. Additionally, sleep deprivation can impair the body’s ability to manage oxidative stress, contributing to increased inflammatory responses. Research indicates that sleep-deprived individuals show elevated levels of various pro-inflammatory cytokines, revealing the depth of this relationship. Moreover, even acute sleep disruptions can provoke an inflammatory response. Understanding these underlying processes is important in addressing health issues holistically. By targeting the improvement of sleep, a potential method for ameliorating inflammation-related health problems emerges.
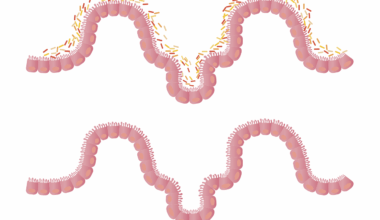
Another area of concern is the bidirectional relationship between inflammation and sleep. When individuals face chronic diseases characterized by inflammation, sleep often suffers. Conditions such as rheumatoid arthritis and inflammatory bowel diseases can lead to increased discomfort and restlessness at night. As such, patients with these conditions frequently report higher instances of poor sleep quality, creating a cycle of suffering. Physicians treating patients with inflammatory conditions recognize the importance of addressing sleep issues. The management of sleep quality often becomes an integral part of treatment regimens due to its direct effects on recovery. Patients are encouraged to be proactive about their sleep in managing symptoms. Recommendations sometimes include sleep hygiene education and cognitive-behavioral therapy. This comprehensive approach aims not only to reduce inflammation but also to restore restorative sleep. Studies show that better sleep contributes positively to symptom management, showcasing the importance of adapting strategies. Health practitioners are exploring various interventions tailored to individual needs, recognizing the distinct challenges faced by those with chronic inflammatory diseases while focusing on improving sleep quality.
Looking Ahead: Future Research Directions
Future research in the field of sleep and inflammation holds great promise. As our understanding deepens, better prevention and treatment strategies can be developed. Addressing the sleep-inflammation link can lead to innovative approaches in managing chronic diseases. Research is increasingly focusing on personalized medicine, where treatment plans consider individual sleep patterns along with inflammatory profiles. Investigating the genetic basis of sleep disorders and inflammation can also provide valuable insights. By identifying biomarkers associated with sleep and inflammation, more targeted therapies may be devised for patients experiencing these issues. Additionally, the impact of sleep interventions on inflammation-related outcomes warrants further exploration. More comprehensive studies that assess diverse populations will yield crucial data on how these relationships function under different circumstances. Furthermore, collaborations among healthcare providers, sleep specialists, and researchers could lead to more integrated approaches to healthcare. The potential benefits of such interdisciplinary efforts may lead to improved patient outcomes while addressing the intertwined challenges of sleep and inflammation comprehensively. Commitment to advancing knowledge in this realm represents a vital step toward enhancing overall health outcomes.
In conclusion, recognizing sleep disruption as a critical marker for inflammatory diseases is essential for advancing healthcare practices. As more individuals and healthcare providers understand the relationship between sleep and inflammation, proactive measures can be taken to improve health outcomes. Prioritizing sleep hygiene, addressing lifestyle factors, and understanding personal sleep needs can lead to better inflammation management. The exploration of the sleep-inflammation connection creates a more holistic approach to patient care, ensuring that chronic diseases are managed effectively. Discussions surrounding sleep should not only occur in the context of mental health but also in physical health realms. Awareness and education on the inflammatory responses to sleep disruption can lead to meaningful changes in treatment paradigms. It is also vital for communities to support initiatives promoting better sleep awareness and education, reducing stigma surrounding sleep issues. Engaging in collective efforts may enhance overall public health by reducing the burden of inflammatory diseases. As we continue to explore this relationship, the integration of sleep science into broader health contexts will undoubtedly prove beneficial in addressing chronic conditions effectively.
This conclusion reflects our understanding of the relationship between sleep and inflammation. With further study and collaboration, our approach to healthcare could evolve significantly, emphasizing sleep’s critical role. Targeting sleep problems can help manage inflammation levels and improve health outcomes significantly.